|
|
|
|
APA PsychNews - CMS Approves Permanent Coverage of Audio-Only Telehealth Services for Mental Illness/SUDs (11-12-21) CMS has expanded the definition of telehealth services that will be permanently eligible for reimbursement under Medicare to include audio-only services for established patients with mental illness/substance use disorders (SUDs) who are unable or unwilling to use video technology. The APA and CPS advocated for these changes (CPS letter available here). The services have been temporarily reimbursed during the COVID-19 public health emergency, but the 2022 Medicare Physician Fee Schedule makes it permement when it goes into effect in January 2022. For additional information see the final rule here, future APA PsychNews articles, and this summary of key points. |
May 12, 2021
Change Is the Only Constant
By Claire Zilber, MD, DFAPA
CPS President
In this, my final President’s letter, I focus on change in several contexts: alterations in psychiatric health as a result of COVID-19, mutations in the virus itself over the course of the last 18 months, policy shifts we need to make to approach universal vaccination, and adaptations we are starting to make as we cautiously emerge from isolation.
The deleterious effect of the pandemic and of SARS-CoV-2 infection on mental health has been well documented in the medical and lay press, and in previous CPS COVID-19 emails. This retrospective EHR review of 236,379 patients who had recovered from COVID-19 found an incidence of a neurological or psychiatric diagnosis in 34% of patients, and a 13% incidence of a new neurological or psychiatric diagnosis in the aftermath of infection. These rates were higher among patients who were admitted to the ICU. Of particular concern is an almost 3% incidence of psychosis, as well as a 19% incidence of anxiety. In the population at large, even without a formal new neuropsychiatric diagnosis, few of us are thriving. Several of my patients and family members were eager to discuss this article on languishing, which explains the “blah” so many of us feel at this point in the pandemic.
Our daily “blah” is punctuated by occasional breezes of excitement, blown in by the wider range of behaviors we now allow ourselves. I hugged a friend! I’m planning a road trip! Going to the grocery store is less scary. As mask mandates are relaxed or lifted entirely in Colorado, depending on the county and setting, concern about variants leaves some people squeamish about reentry. Such anxiety may have been exacerbated by news that a variant initially identified in India has been found in Mesa County. You might assuage that fear by watching this highly scientific and reassuring 10-minute video on vaccines and variants. If you have been vaccinated, and by now I hope all CPS members have achieved this milestone, you are part of the solution.
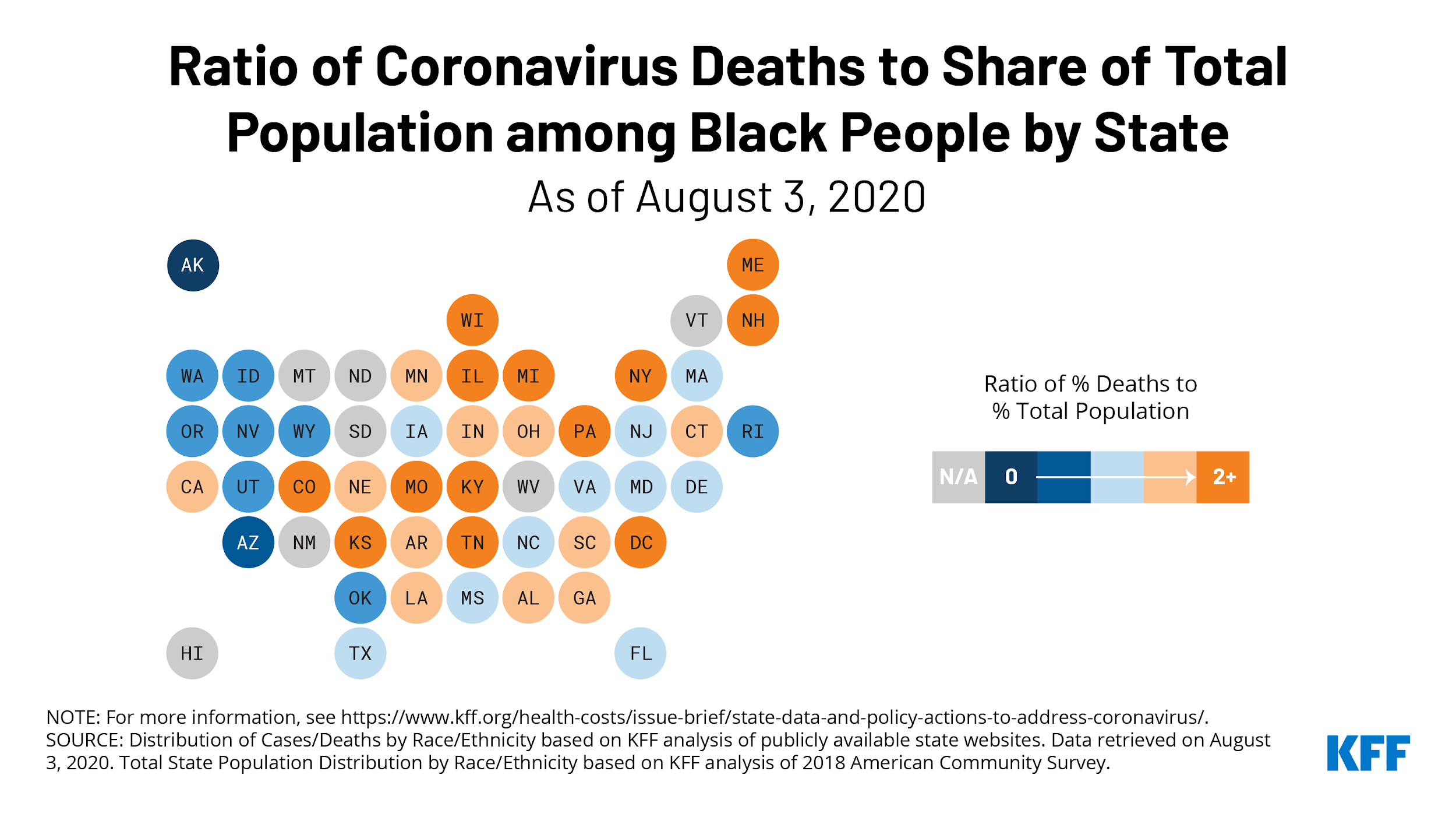
More than two million people in Colorado have been fully vaccinated against COVID-19, which represents over a third of our population. This is consistent with overall US vaccination rates. Supply now outstrips demand, yet Black and Hispanic communities remain underrepresented among the vaccinated (click on the Demographics button at the top link in this paragraph to see the Colorado data), a result of mistrust engendered by racism in healthcare as well as remediable problems with vaccine access.
Meanwhile, as rich countries succeed at vaccinating their populations, developing countries lag far, far behind. "Nearly 900 million vaccine doses have been administered globally, but over 81% have gone to high- or upper middle-income countries, while low-income countries have received just 0.3%," WHO Director-general Tedros Adhanom Ghebreyesus said on April 23, 2021. Similarly, climate activist Greta Thunberg decried vaccine inequity as unethical. It is simultaneously thrilling and obvious that a teenager would scold the world about justice. It is imperative that the United States share our vaccine technology and stockpiled doses with developing countries whose people are suffering the most, such as India and Brazil. The BBC has an excellent global COVID map for those of you who want to dig into the disparities in cases, deaths, and vaccinations. Towards the bottom of that web page you’ll be riveted by an animated graph of the geographic spread of cases from February 2020 to the present.
Our gratitude about being fully vaccinated with highly effective mRNA vaccines may be slightly tempered by shame about our privilege, just as our relief and joy at being able to emerge from our tight pandemic bubbles may be subdued by anxiety about how far to go in relaxation of protocols. The CDC guidance allows fully vaccinated people from two separate households to remove their masks in private settings. However, the Colorado Department of Public Health and the Environment (CDPHE) continues to mandate masks in healthcare settings, including outpatient offices, even if everyone in the room is fully vaccinated. One might argue that a solo psychiatrist’s private practice office is closer to a living room in terms of exposure risk, yet even so called “limited healthcare settings” like audiology and occupational therapy practices are required to continue to conduct appointments by telehealth whenever possible and wear masks when in person.
I am aware that some of us have returned to in-person appointments when the patient and professional are both fully vaccinated. Just know that you are deviating from public health guidance when you do this unless you and your patient are both wearing masks. A lot depends on the size of the building that houses your office, the nature of the ventilation, and the number of other people in the building. If you want to delve into engineering models of airborne risk, see this MIT analysis. For additional scientific guidance about indoor settings, this online app calculates the risk of being in a variety of spaces (ie: office, classroom, commercial airliner, etc), for a variety of minutes/hours, in a variety of conditions (ie: masks, no masks, speaking, exercising, singing). It is mostly reassuring, and it also reinforces the value of continuing to wear masks in indoor public spaces. Be sure to adjust the room specifications to fit your clinical setting and select the B.1.1.7 strain, which as of mid-April was the dominant strain in Colorado. Even if you see one patient at a time in a building with moderately good ventilation, if you see eight individual, consecutive patients in a day, you may be placing yourself and your patients at risk if you aren’t both wearing masks. Because I am a risk-averse rule follower, I continue to see my patients exclusively via telehealth, although I am moving that activity back to the office this week.
Emerging from what I hope has been the worst of the pandemic, it is natural to wonder about the impact of these terrible times on ourselves and society. This thoughtful article employs the most famous novel by my favorite author, Jose Saramago, as an allegory for COVID-19. I am optimistic that our collective ingenuity in adaptation will bring forth from the recent horrors of the pandemic and social upheaval innovations in healthcare delivery, social justice, clean energy, food and housing security, and immigration policy that will have a lasting positive change on the populace and the planet.
As I pass the gavel of responsibility for CPS leadership into the capable hands of Dr. Aaron Meng, I reflect on the experience of serving as president during the pandemic. I am grateful that I had the opportunity to be so strongly connected to my professional community, giving me a sense of purpose and collegial companionship during a year of isolation. Although the lyrics aren’t a perfect fit, the gratitude expressed in this uplifting acapella video, Change in My Life, feels like a fitting way to say farewell.
Colorado Psychiatric Society COVID-19 Resource List
May 12, 2021
|
|
The APA Committee on Disaster Psychiatry - COVID-19 Pandemic Guidance Document ACTIONS AND ACTIVITIES THAT A HEALTHCARE ORGANIZATION CAN TAKE TO SUPPORT ITS PHYSICIAN WORKFORCE WELL-BEING DURING COVID-19 AND BEYOND (download)and COVID-19 Pandemic Guidance Document REINTEGRATION OF HEALTHCARE WORKERS FOLLOWING COVID SERVICE (download) |
|
Last chance - closes May 15th! CPS/APA - Help CPS and APA Fight for Better Reimbursement for YOU – Take our Insurance Survey! Help us advocate on behalf of psychiatrists to increase reimbursement and decrease administrative burdens from public and private payers. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
April 7, 2021
This Sadistic Ultra-Marathon
By Claire Zilber, MD, DFAPA
CPS President
April 7, 2021
Happy Spring! Last April we thought we were in a sprint, by summer we realized it was a marathon, and now, with the promise of vaccines and the peril of new variants, it looks like we’re in a sadistic ultra-marathon for which the organizers won’t disclose the length of the course. This is especially true in light of this commentary from the Lancet about a Danish study of reinfection with SARS-CoV-2. Immunity from SARS-CoV-2 infection is not as robust as immunity from vaccination, so herd immunity may not be realizable without global vaccination. In this letter I will provide updates about vaccination, consider the ethics of vaccination passports, focus our attention on two neglected populations of vulnerable individuals, and highlight new information about neuropsychiatric and psychosocial sequelae of the pandemic.
The CDC issued new domestic and international travel guidelines on 4/2/21 for people who are fully vaccinated. Listen to this brief, thoughtful interview with Jeanne Marrazzo, MD, Director of Infectious Disease at University of Alabama School of Medicine, focused on balancing optimism about vaccination with caution about ongoing infections. She encourages us to focus on community health rather than merely considering personal health.
Once we each have our vaccination cards in hand, what should we do with them? Are they the same thing as a vaccine passport? This piece discusses the history of vaccination cards and the possible importance of the current one. They might become linked to a vaccine passport, but that has become a highly controversial concept. This NEJM paper considers both the political and ethical implications of vaccine passports, which may confer privilege in an inequitable manner and create a “mandate” that inadvertently de-incentivizes voluntary vaccination. This nuanced PBS story goes into more depth about the concept of vaccine passports, their near certainty for international flights, concerns they raise about healthcare privacy, and their potential use as a divisive political weapon.
Colorado is doing fairly well with our vaccinations, ranking 24th among the states in percentage of population fully vaccinated. However, as seen across the country, white Coloradans represent a disproportionate share of those vaccinated despite being at lower risk of clinically relevant infection. The ethnic group faring even better than Caucasians in vaccination rates are Native Americans. As detailed in this report, 21.8% of Indigenous Americans had received at least one dose of vaccine last week, compared to 21.3% of white Americans. Some tribes are taking the lead on vaccinating their nations, and in South Dakota the Sioux are being vaccinated at twice the rate of other people in that state because of the efforts of the Indian Health Service (IHS). Despite historical underfunding of the IHS, it appears to be meeting the challenge of the moment. Unfortunately, Native Americans living in urban areas who are not already registered for health care services with the IHS are finding it difficult to obtain a vaccine.
In addition to racial and ethnic minority groups, there are other populations that have received less notice in the pandemic despite the fact that they, too, have increased medical and psychosocial vulnerabilities, among them those with intellectual disabilities and the LGBTQ population. As detailed in this large population study, intellectual disability is the strongest independent risk factor for COVID-19, and confers the third highest mortality rate. This is partly because of higher medical comorbidities in this population, and because of greater exposure through group living and interaction with home care aides. People with intellectual disabilities have had their lives profoundly disrupted by the pandemic because of the loss of day programs, as detailed in The Arc’s briefing paper and the COVID-19 resource page on its website. Isolated, lonely, disoriented without their routines and regular social/therapeutic interactions, intellectually and developmentally disabled people may have more difficulty adapting to the pandemic than the rest of us. We need a better pandemic plan than “shelter at home” for these populations.
Another group that faces higher risks from COVID-19 because of a greater incidence of health comorbidities is the LGBTQ population. This MMWR report documents the higher adjusted prevalence of asthma, cancer, heart disease, COPD, hypertension, kidney disease, obesity, smoking, and stroke in sexual-minority populations than in heterosexual persons. In addition, this Kaiser Family Foundation analysis documents the disproportionate burden of job loss and mental health stress on LGBT individuals compared to non-LGBT people. Furthermore, pandemic isolation and school closures are distinct misfortunes for queer and trans youth, who already faced higher rates of mental illness before the pandemic, now exacerbated by loss of social networks and support. Especially for youth sheltering at home with unsupportive or abusive family members, the peril to their safety is tangible.
The neuropsychiatric and psychological effects of COVID continue to reveal themselves. Several possible mechanisms of brain injury from COVID are postulated, from direct invasion of the CNS by SARS-CoV-2 (for which there is not yet definitive evidence); to neurotoxicity from inflammatory cytokines, increased glutamate, and upregulation of NDMA receptors; to micro-strokes from endothelial damage. An internet-based survey identified an association between severity of acute COVID symptoms, especially headache, with later symptoms of depression. An alarming 52% of the 3900 respondents reported current symptoms of major depression, on average four months after being ill with COVID.
As described in previous COVID emails, there are consistent reports of increased anxiety and depression among people who have not developed COVID. In my practice, I have seen two cases of new onset agoraphobia as a result of the pandemic. One developed in a patient with preexisting generalized anxiety disorder who had his first-ever panic attack in a grocery store last spring, after which he has experienced enduring agoraphobia. The other patient has a preexisting diagnosis of post-traumatic stress disorder and had not been agoraphobic until the pandemic. In both patients, catastrophic cognitions lead to avoidance behaviors. This study validates a new research tool to assess catastrophic cognitions about SARS-CoV-2. A European study of the impact of the pandemic across psychiatric disorders compared with healthy controls found increased symptom severity in subjects with depression, body dysmorphic disorder, illness anxiety disorder, and generalized anxiety disorder. A CDC study identified increases in anxiety and depression throughout the course of the pandemic, especially among young adults and those with less than a high school education.
Even for people without underlying mental health disorders, the pandemic has had a profound effect on stress and behavior. I notice myself yearning to hug friends, fly to visit family members, and eat in a restaurant again while simultaneously avoiding planning any of those activities, even for a time after I receive my second dose of vaccine. In that context, I appreciate this article about how pandemic fatigue has made us withdraw from others, and the author’s encouragement to reach back out again when we feel ready while also honoring our need for “aloneness.” Even if you don’t want to read the whole article, read the poem by Donna Ashworth. The permission to feel what we feel and the sense that we are not alone in these feelings is supremely soothing.
Colorado Psychiatric Society COVID-19 Resource List
April 7, 2021
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
Thank you to our Platinum Partner for their support
March 10, 2021
Pandemic Equipoise
By Claire Zilber, MD, DFAPA
CPS President
March 10, 2021
We are at a point of equipoise, balancing precariously between opposing forces. Global COVID cases are rising after having fallen for six weeks. We have three amazing vaccines, yet a mere 10% of the population has been fully vaccinated. ICUs are no longer overwhelmed, but long-term consequences of COVID are becoming more apparent. This email will focus on maintaining safe behaviors while the vaccination effort continues, offer updates about delirium in COVID and post-COVID syndrome, and consider loneliness and forgiveness as crucial experiences in the pandemic.
As some states lift mask mandates and bar & restaurant restrictions, we can expect to see a fourth surge in the US. In contrast to some governors, the CDC advises us to double mask, wearing a cloth mask over a medical procedure mask, to reduce the spread of SARS-CoV-2. This MMWR report has an instructive graphic. I don’t feel the need to do this while walking my dog, but I’ve started double masking when I go to the store or any indoor appointment. The CDC has also issued guidelines for those who have been fully vaccinated, distinguishing the situations in which being indoors unmasked may be safe from those where masking and social distancing is still advised. Here is the science brief behind the new guidelines. Before gathering with others, especially if you plan to be unmasked, consider self-administering an at-home molecular SARS-CoV-2 test. The first FDA approved home test kit uses a nasal swab, cartridge reader and mobile app, and delivers results in about 20 minutes.
Vaccines are here and, as of March 7, 1,054,537 Coloradans have received at least one dose and 612,538 have been fully vaccinated. Our state has an estimated population of 5.94 million, which means around 10.3% of Coloradans are fully vaccinated. In my last COVID-19 email, I discussed inequities in vaccine access and advocated for vaccination clinics in community mental health centers (MHC) to reach our vulnerable patients with serious and persistent mental illness. A convenience survey of three Denver metro area MHC leaders revealed that this had already begun. MHCD (Denver), Jefferson Center for Mental Health, and Community Reach Center (Adams County) each have an onsite vaccination clinic for eligible age and comorbidity groups managed by their pharmacies. (If someone has time on their hands, a survey of all the other county MHCs would be enlightening.)
Case rates and hospitalizations are down, but they are not over. Even when the virus is contained, there will still be a need for a healthcare response to the COVID-related fallout.
As psychiatrists, we know the pandemic of PTSD and other psychiatric disorders unleashed by COVID is only just beginning. According to an Italian study, delirium is a risk factor for developing PTSD, as are female gender and the presence of psychiatric comorbidities. The prevalence of PTSD in this sample of 381 consecutive patients was a shocking 30.2%. An international study of over 2000 patients in ICUs with COVID-19 found that almost 55% had delirium lasting a median of 3 days. Mechanical ventilation; use of restraints; infusions of benzodiazepines, opioids, and vasopressors; and antipsychotics were each associated with a higher risk of delirium, whereas in person or virtual contact with family members was associated with a lower risk of delirium. With this knowledge, C/L psychiatrists may have the opportunity to avert PTSD by avoiding or reducing delirium.
Even in patients with mild or asymptomatic infection, long term sequelae are common. A study of adults six months after COVID infection found that over a quarter of patients reported persistent symptoms, with fatigue, loss of smell or taste, and brain fog as common complaints. It is easy to imagine the negative impact of these long-term symptoms on one’s quality of life and sense of wellbeing. Another study examined post-COVID symptoms exclusively in patients who had been asymptomatic with their acute infection, and found that nearly a third of patients across all age groups developed chronic symptoms. Although scientists cracked the code of the viral genome and developed vaccines in record time, we still have so much more to learn about this virus, its effect on the body, and how to help people recover.
The COVID-19 pandemic has created a second, mental health pandemic that may outstrip our traditional treatment resources. In addition to PTSD, anxiety disorders, depressive disorder and substance use disorders, the last year of social distancing has uncovered a preexisting epidemic of loneliness. I am intrigued by this report on training laypeople to provide empathetic phone calls to homebound older adults. This is a low-cost, scalable option that seems to be beneficial. Might this be an innovation for our overtaxed mental health resources even after the pandemic? What if we launched a public health campaign that taught kindness, compassion and outreach to citizens? The UK has a Minister of Loneliness. Shortly before the pandemic, a US survey found that three in five people here are lonely. Does the US need a similar person or office to respond to the public health implications of so many lonely, fatigued, traumatized people?
Colorado has recorded 5,995 deaths from COVID, or one tenth of one percent of the population. It is likely we each have lost someone, a patient or family member or friend overcome by this virus. While dealing with our own grief, we have helped our patients cope with cascading losses. I have noticed the disparate ways my patients talk about COVID transmission within families. One person steadfastly avoids casting any blame on a sibling for infecting their elderly parents, one of whom died. This person focuses instead on gratitude that the sibling was present to take care of the parents. Another patient is contorted with rage directed at the spouse of an acquaintance. The spouse was careless in masking and distancing and brought infection home to their partner, who had been cautious because of medical comorbidities. The dialectic between blame and forgiveness is movingly captured in this insightful viewpoint titled, “It’s Not Your Fault.” I especially appreciate the closing sentences: “We must find our way quickly to forgiveness, for each other and for ourselves. This story cannot be about shame and guilt.”
Colorado Psychiatric Society COVID-19 Resource List
March 10, 2021
|
|
Colorado Medical Board - Rule 160 - Electronic Prescribing of Controlled Substances - Most prescribers in Colorado will have to use e-prescribing for all controlled substances by July 1, 2021. The law (SB19-079 Electronic Prescribing Controlled Substances) states that solo and rural practitioners will need to comply by July 1, 2023. Companies (such as OptumRx) may have instituted their own timelines and requirements not covered by Colorado Law (2-14-21) |
|
CPS/APA - Survey (deadline 3-15-21) - CPS is thrilled the APA collaborated with us on a nationwide survey to gather information on outpatient psychiatry practices, which will help guide advocacy efforts. We especially need to hear from members who do not accept Medicaid, Medicare or private insurance. Please take a few short minutes to complete the survey and guide your organizations! |
|
APA Annual Meeting - American Psychiatric Association Annual Meeting: Finding Equity Through Advances in Mind & Brain in Unsettled Times) - Featured Lectures + Speakers Dr. Anthony Fauci and Isabel Wilkerson (May 1-3, 2021 Online) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
Thank you to our Platinum Partner for their support![]()
February 2021
Uneven Ground: Vaccination Inequity
CPS President
Having saved all my vacation weeks in medical school for the very end, I was able to travel to Tibet and Nepal. I set out to climb Kala Patthar, an 18,514 foot pile of limestone and shale, from the top of which one has a clear view of Mt. Everest. Because our Sherpas threatened to mutiny so they could attend the Mani Rimdu festival scheduled for the same day as our summit, we shaved two acclimatization days off our ascent. Coming from sea level, I felt drained of energy and struggled for oxygen. I gave myself permission not to reach the summit, but talked myself into taking “just one more step.” The shale sometimes meant a step forward was really a slide back.
Recently, I have been recalling that long-ago climb, applying its lessons to this point in the pandemic. We find ourselves at a precarious place on the pandemic’s path. We have one foot on solid limestone, our hope bolstered by effective vaccines that many healthcare providers and seniors have already received. Our other foot is slipping on the shale of a mutating virus whose new variants are more contagious (UK, Brazil, South Africa and California variants) and more virulent (UK variant), provoking fear of another surge before we have completely emerged from the last one. As we struggle to navigate this terrain, some of us are better equipped than others by virtue of our health status, our ethnicity, our wealth, and/or our privilege. Just as a well-equipped and experienced mountaineer would stop to assist one who may be struggling, it is incumbent upon us to help our more vulnerable neighbors, and especially our most at-risk patients.
According to COVIDActNow, an excellent website with state and county statistics about infection rates, vaccination rates, ICU capacity and more, 9.2% of Coloradans have received their first dose of vaccine, and 3.4% have had both doses. One glaring problem is that these vaccines are disproportionately in the arms of well-off, white people. COVIDActNow doesn’t break down their data by race or ethnicity, but there is evidence of significant disparities in vaccination rates. This Colorado Sun story reports that less than 2% of Coloradans who have received the vaccine are Black, yet Black people represent 4% of the population. An even greater disparity exists in the state’s Hispanic/Latino population: they comprise 22% of Coloradans but only 4.3% of those who have been vaccinated. If anything, these groups should be vaccinated at a higher rate than the rest of the population because they are at more risk of infection, hospitalization and death from COVID. For example, this CDC Morbidity and Mortality Weekly Report reveals that in the first ten months of the pandemic in Denver, the majority of cases, hospitalizations and deaths were among Hispanics, although they represent only a quarter of the city’s population.
This Colorado Public Radio report details why it is not accurate to suggest that most healthcare providers and seniors are white as an explanation for the vaccination rate disparity. This Kaiser Health News report further unravels the myth that the reason fewer Black people have received the vaccine is because most health care workers are white. In part, the lower vaccination rates of Black Americans may be due to vaccine hesitancy, as documented in this Pew Research Report, which shows that only 42% of Blacks express willingness to receive the vaccine, compared to 61% and 63% for Latinos and Whites, respectively. But that data doesn’t explain the low vaccination rates in the Latino population. It is our duty to find ways to overcome this vaccine avoidance by Blacks, not by bullying but by building trust and engagement. It is also our responsibility to understand and remedy the low vaccination rates in Latinos.
The current web-based systems for obtaining vaccination appointments are part of the problem. The elderly and underprivileged may lack the web-connected devices and internet skills with which to make appointments online. To mitigate this problem, CDPHE has held two mass vaccination programs in the San Luis Valley and one on the west side of Denver to reach Latino/Hispanic residents. Many more efforts like this will be needed. Pop-up vaccination events at predominantly Black churches and barbershops, at Native American health and cultural centers, and other trusted sites in Black, Indigenous and People of Color (BIPOC) communities are necessary to ensure justice in the vaccination effort. Otherwise, we will continue to see reports, like this one, that those who live in wealthy, white neighborhoods are receiving the vaccine ahead of others. Equally appalling are the stories about wealthy citizens of other countries flying to Miami, Houston and San Diego for COVID vaccines. I have heard that some have flown to Denver, driven to a church outside of Vail, and received their vaccines there. Those vaccines were intended for low-income workers. I am disgusted.
We don’t like to think that racism has infiltrated into healthcare, but it has been as deeply entrenched in medical settings as anywhere else. From the grossly unethical Tuskegee syphilis study, to the appropriation of Henrietta Lacks’ cervical cells for research without her consent, to the uneven distribution of medical resources and procedures in the US, to overt racism in clinical encounters, racism in healthcare is a profound problem that should concern and involve all of us. This recent NEJM Viewpoint, “One of Us”, about how racism affects Black healthcare providers, is especially poignant. I am inspired by stories like this one, about individual healthcare providers finding ways to fill the gaps in underserved neighborhoods. We need to amplify these efforts, to make them universal rather than dependent on a specific individual possessed of abundant initiative. The Colorado Vaccine Equity Task Force aims to provide accurate information, knowledgeable speakers, and vaccination events to BIPOC communities. Their goal is to see 80% of Colorado BIPOC adults immunized by autumn, 2021.
As psychiatrists, we may be best situated to bring the vaccine to another population that experiences health disparities and reduced access to medical services: those with chronic mental illness (CMI). A recent study of COVID-19 mortality found that schizophrenia spectrum disorders conferred the second greatest risk, behind age, of COVID-19 mortality. Patients with schizophrenia spectrum disorders were 2.67 times more likely to die from COVID-19 within 45 days of testing positive than individuals with no mental illness. A pre-pandemic study of an intervention to address vaccination disparities for the CMI population demonstrated that creating a vaccination clinic in a community mental health center (CMHC) increased the vaccination rate from 18.75% to 83%. This remarkable success rate points to the potential for creating pop-up vaccination clinics at CMHCs to reach our most vulnerable patients. I hope that CPS and the APA will help advocate with CDPHE and the CDC, respectively, for this kind of innovation to reduce healthcare inequities among our patients, especially our CMI patients who are from BIPOC communities.
In addition to advocating for and organizing vaccination events that are more geographically and culturally accessible to the full spectrum of humanity in Colorado, psychiatrists may also want to examine the ways in which we unwittingly continue to exercise our privilege at others’ expense. This NYT op-ed by a former ER doctor turned journalist discusses those who have “jumped the line.” She says, “Pity the rule followers: Many older Americans who are not tech-savvy or lack internet access have been unable to get [appointment] slots.” Neither of my parents has had a first dose yet despite the fact that they can navigate the internet. I admit that if they lived in Colorado, I might work my connections to find them a place in line (to which they are fully entitled anyway because of their age). But another part of me thinks that’s unjust. My parents have the privilege of wealth, excellent nutrition, and overall good health. I should really be helping seniors who have fewer resources, those who struggle to buy fresh produce, pay the utility bills, and afford their medications.
Another important element of our response to the exercise of privilege in jumping the vaccination line is to educate the public and our patients about the ethics of vaccine distribution. They key point is the principle of justice in health care, which posits that resources should be allocated with systematic fairness. This viewpoint article from the NEJM offers a clear, nuanced ethical analysis of why politicians getting their vaccinations in advance of the elderly and those on the front line is an injustice.
In his paper, What Will White Psychiatrists Sacrifice?, Dr. Keith Gallagher admits, “I have shrugged my shoulders at injustice as if I were powerless to influence it.” He asserts that we must make sacrifices to right the wrongs from which we have benefited, which involves recognizing and ceding our privilege. This may mean different things for each of us. For me, this includes not getting my vaccine ahead of the general public, while advocating consistently to help my senior and/or medically vulnerable patients get theirs. I continue to explore the other ways I can give up parts of my privilege to help raise up those who struggle more than I have ever needed to do. It will mean more than making financial contributions, although those are important. It will mean being willing not to reach the summit of this trail until the entire hiking party reaches it with me.
We have been on this very steep trail for almost a year. We are exhausted. It looks like the trail may be leveling out up ahead. Don’t drink all your water and finish your trail mix yet! This is likely a false summit, and we may have miles and months ahead of us. I did make it to the top of Kala Patthar, but it wasn’t easy. I took “just one more step,” one step at a time, all the way up that heap of rocks. The view was spectacular.
Much gratitude to Beth Cookson, MD, for sharing “One of Us” by Raymond Givens, MD, PhD.
Colorado Psychiatric Society COVID-19 Resource List
February 2021
Updates |
|
HHS - Public Health Emergency Expected to be Extended Through 2021 (download) - The U.S. Department of Health and Human Services (HHS) has communicated through a letter to Governors it will likely extend the Public Health Emergency (PHE) in 90 day increments through 2021 |
|
CPR - Colorado Opens COVID-19 Vaccine Hotline - The state is launching a hotline to help Coloradans get answers to questions about COVID-19 and vaccinations - 1-877-CO-VAX-CO or 1-877-268-2926 |
|
APA - Learn More and Register - Registration is now open for APA's online 2021 Annual Meeting Finding Equity Through Advances in Mind and Brain in Unsettled Times, which will be held Saturday to Monday, May 1 to 3. National Institute of Allergy and Infectious Diseases Director Anthony Fauci, M.D., will deliver the William C. Menninger Memorial Convocation Lecture on Sunday, May 2. $275 early registration (before March 1st), $375 standard registration. |
|
|
|
|
JAMA - Trends in US Emergency Department Visits for Mental Health, Overdose, and Violence Outcomes Before and During the COVID-19 Pandemic - These findings suggest that ED care seeking shifted s during thea pandemic, underscoring the need to integrate mental health, substance use, and violence screening and prevention services into response activities during public health crises (2-3-21). Also see Nature - COVID’s Mental-Health Toll: How Scientists Are Tracking a Surge in Depression - Researchers are using huge data sets to link changes in mental health to coronavirus-response measures (2-3-21) |
|
KOAA Southern Colorado - Growing number of pregnant women, new mothers seeking mental health resources during COVID-19 pandemic - Quotes CCAPS members Celeste St. John-Larkin and Anastasia Klott (1-21-21) |
|
JAMA - Virtual Care, Telemedicine Visits, and Real Connection in the Era of COVID-19 Unforeseen Opportunity in the Face of Adversity (2-2-21); and Journal of General Internal Medicine - The Transition to Telehealth d)uring the First Months of the COVID-19 Pandemic: Evidence from a National Sample of Patients - Mental Health and Substance Use Disorders the Most Common Telehealth Appointment (1-6-21) |
|
JAMA - Vaccine Distribution—Equity Left Behind? (1-29-21) |
|
NYT - The Science of Reasoning With Unreasonable People - Don’t try to change someone else’s mind. Instead, help them find their own motivation to change (1-31-20) |
|
Denver Health Volunteer Opportunity - Volunteers page - DHHA is soliciting individuals with clinical backgrounds that can fill positions specific to reconstituting medication and administering vaccines to support the need to increase capacity at the following vaccination clinics; Pavilion C, Peña, Lowry, West. |
| APA - Members Can Now Order PPE Through Project N95 Anytime - Vetted PPE through Project N95 is now available for APA members on an ongoing basis |
|
|
Wired - It’s Not Just You: Everyone’s Mental Health Is Suffering - If you’re thinking, “Oh, I just need to suck it up,” stop. What you’re feeling is real. Here’s how to cope (1-18-21) |
|
CNN - The rise of the fake commute, and why it's good for your mental health (1-18-21) |
|
CPR - Coloradans Will Not Need ID To Receive COVID Vaccine In Colorado, COVID-19 vaccine providers cannot require people to have proof of identification in order to be inoculated - Colorado providers can still ask people to give their name, age and address, but those requests cannot dictate whether or not the person will be vaccinated (1-19-21). Also see Center for Health Progress - COVID-19 Vaccine FAQ for Immigrants in Colorado in English or Spanish. |
| Denverite - Denver got nearly $22 million in federal money for emergency rental assistance. Here’s how you can start applying for some of it - The money will be administered by the city’s Department of Housing Stability with help from local nonprofit organizations - call 311 and select option 6 (1-26-21) |
|
The Colorado Sun - “Hug tent” allows for safe family embraces at Colorado home for the elderly - The tent set up outside Juniper Village at Louisville allowed family members to connect through a 4-millimeter-thick clear plastic barrier (2-5-21) |
|
HCFP - Non-Emergent Medical Transportation (NEMT) - NEMT is a Health First Colorado benefit for Colorado Medicaid members who don't have transportation to medical appointments. It can be used to help patients get vaccinated when they are eligible. NEMT is provided through one transportation broker, IntelliRide. Members and assistors can contact IntelliRide at 1-855-489-4999 or 303-398-2155 (State Relay: 711) or visit their website for more information |
|
CHI - The Pandemic Behind Bars - COVID-19, Vaccination, and the People in Colorado’s Prisons and Jails - More than 16,000 people have contracted COVID-19 as part of outbreaks at Colorado prisons, jails, and other detention facilities, according to an analysis of state and federal data by the Colorado Health Institute (CHI) (1-28-21) |
|
CPR - On The Fence About COVID Vaccines? These Teens Want To Talk To You - Colorado high schoolers are combining empathy and scientific truth to produce videos aimed at persuading hesitant people to get vaccinated (2-3-21) |
|
The Colorado Sun - Fentanyl overdoses are surging in Colorado as the powerful opioid is disguised as other drugs (2-4-21). Also see Fox31 - Warning: Fentanyl found in street drugs in Boulder County (2-8-21) and Denver7 - Boulder County Health warns about another batch of fentanyl-tainted drugs being sold on the street - Tainted drugs leading to increase in overdoses (2-6-21) |
|
Slate - All the Presidents’ Pets - A cat named Miss Pussy. A virulently racist parrot. A pair of possums, which were later eaten for dinner. All the best—and worst!—presidential pets in American history, ranked (1-31-21) |
|
NYT - Why You Should Brave the ‘Bad’ Weather - My British upbringing taught me that socializing outdoors shouldn’t stop when rain falls and temperatures drop (11-7-20) |
|
NYT - Surge of Student Suicides Pushes Las Vegas Schools to Reopen Firmly linking teen suicides to school closings is difficult, but rising mental health emergencies and suicide rates point to the toll the pandemic lockdown is taking (1-24-21) |
|
CDC - New Toolkit for Pregnant People and New Parents - The CDC’s latest COVID-19 resource offers information on pregnancy, breastfeeding, and caring for infants during COVID-19 (2-8-21) |
|
NYT - The Primal Scream, a series that examines the pandemic’s effect on working mothers in America. America’s Mothers Are in Crisis - Is anyone listening to them? Its not just the working from home, the record unemployment or the remote schooling. This is a mental health crisis too. Also see This isn’t burnout, it’s betrayal - a psychiatrist suggests ways moms can fight back when the system is stacked against them - Includes suggestions on what to do including recognizing that these problems are systemic (2-4-21) |
|
Psychiatric Times - Suicides in Vulnerable Populations During the COVID-19 Pandemic (6 minute video) - Early data out of Maryland suggests that suicides during the initial COVID-19 wave actually dropped, compared to previous years. At the same time, Nestadt’s research also found that suicide rates among Black Marylanders rose sharply (1-19-21) |
|
USA Today - Black trans people are struggling to find therapists after a tough year, but these non-profits are taking action - includes links to organizations that support the Black transgender community such as Fearless Femme 100, a project to provide free mental health care to QTBIPOC in response to the COVID-19 pandemic (1-27-21) |
| 9News - 'A process of listening and hearing': Task force aims to address minorities' vaccine concerns - A statewide survey in September showed nearly 50% of Black and Latino Coloradans would not get the COVID-19 vaccine (1-20-21) |
| El Pais - A room, a bar and a classroom: how the coronavirus is spread through the air - The risk of contagion is highest in indoor spaces but can be reduced by applying all available measures to combat infection via aerosols. Here is an overview of the likelihood of infection in three everyday scenarios, based on the safety measures used and the length of exposure (updated link and article) |
| Recovery Review - Loneliness in the pandemic: risky times (1-24-21) |
Key Resources |
|
|
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
February 3, 2021
Colorado Psychiatric Society COVID-19 Vaccine Update
February 3, 2021
|
|
Colorado is currently vaccinating eligible Coloradans for Phase 1A and Phase 1B.1. Governor Polis announced that Colorado is now able to expand vaccine eligibility and begin the next stage of Phase 1B (known as Phase 1B.2). Coloradans in Phase 1B.2 will be eligible beginning February 8. See the updated vaccine phase table and the vaccine distribution phase update FAQ (both updated 1-29-21) for more information. |
|
In addition to the health care workers, long-term facility staff, and Coloradans ages 70+ who are already eligible, beginning February 8, Colorado will begin vaccinating the following people:
|
|
|
The Colorado Medical Society launched a new partnership with Children's Hospital Colorado and the Colorado Department of Public Health and Environment with the focus to get "shots in the arms" of any remaining Phase 1A or 1B physicians or other front line health care worker that have yet to be vaccinated. Sign up here. |
|
If you or someone you love is 65 or older, click here for information on where you can get vaccinated in Colorado and how to sign up. |
|
If you are eligible and having trouble accessing a vaccine, please contact CPS and we will do our best to assist you. |
January 20, 2021
Vaccines are on Everyone's Mind
By Claire Zilber, MD, DFAPACPS President
We are at a difficult and dangerous phase of the pandemic. With vaccines available to some but not most, there is a risk that people will relax the stringency of their safety behaviors, wear masks less consistently, take more liberties with social exposure, and generally behave like the peril has passed. This letter will describe the state of Colorado’s vaccination effort, provide the most recent information about vaccine availability, discuss vaccine reluctance and how to work with people who have fears about its safety, and illuminate the human vulnerability to conspiracy theories that have tainted the vaccine effort.
CMS held a Town Hall on vaccines on Wednesday, January 13, with presentations by Dr. Eric France (CMO of CDPHE), Dr. Mark Johnson (CMO of Jeffco Public Health) and Dr. Darlene Tad-y (VP of clinical affairs for Colorado Hospital Association). Colorado has 5.8 million residents, which represents 1.69% of the US population. We receive a proportionate number of vaccine doses from the US supply. Although we have the capacity to deliver more doses per week than are currently being administered, we don’t have more doses. We were told in the Town Hall that this would change this week or next, as the administration releases the vaccines that are being held in reserve for second doses. However, last Friday we learned that the federal government has no vaccines in reserve. As of last week, Colorado has received approximately 500,000 doses of the vaccine, and has immunized 209,000 people with one dose and 44,000 with two. At his press conference yesterday, Governor Polis announced that 5% of the state’s population will have received a first dose by the end of this week, including 20% of people over 70.
The Town Hall addressed the somewhat disorganized process of moving from 1a to 1b categories (scroll down to chart of Phases) for vaccination, shifting from hospital-based to community-based vaccinations, which Dr. Tad-y framed as “building the plane after it’s already taken off.” It is reasonable to move away from hospitals as the primary location for vaccination, as hospitals are struggling to staff vaccination clinics while in the midst of a COVID surge. Furthermore, in rural counties there are practical geographic reasons to use pharmacies rather than hospitals for vaccination.
The information about which sites are open for vaccination is changing weekly, sometimes daily, so practicing patience will help us contend with the resulting frustrations. Depending on the county in which a person resides, there are different places administering the vaccine. This webpage lists those places by county. For people who are unable or unwilling to go online, COHELP is a phone line that answers vaccine questions in multiple languages: 1-877-462-2911. A person may sign up through the patient portal of each system in their county and then wait for an invitation to schedule. There is an option to sign up by phone, but wait times can be as long as three hours. Anyone who gets a first dose is automatically scheduled for a second dose at the same location. Kaiser, UCHEALTH, Centura, and all the other major health systems are administering vaccines to 1a and the first half of the 1b list (above the dotted line on the chart) which includes seniors over 70, HCPs who work in person with patients who are not known to be COVID positive, firefighters, police, correctional workers and funeral workers. In addition, two major pharmacy chains that have outlets throughout the state (Safeway is one; the second may be King Soopers but they weren’t named at the time of this writing), will begin administering vaccines to people 70 and older.
Counties are allocated doses of vaccine based on their population. It is disruptive to the fairness of the distribution process if a person with a second home in a different county gets their vaccine in the county of their second home. Please discourage this behavior.
The state’s goal is to complete the vaccination of people aged 70+ by the end of February. Everyone appreciates that this vaccine is a precious resource and doses are not being wasted. If someone doesn’t show for their vaccine appointment, the remaining dose is put into someone else’s arm even if that person is not in the 1b category.
Currently, the state is receiving the Pfizer/BioNTech and Moderna vaccines, both of which require two doses. Additional vaccines by Johnson&Johnson, AstraZenica and Novavax are in Stage 2-3 clinical trials. The first two will be single-dose vaccines, while the Novavax will likely require two doses.
Although we are currently focused on getting the vaccine to people who desperately want it, we must also focus on those who are more reluctant, particularly people whose communities are most hard-hit by COVID. This study found that the proportion of adults who said they were somewhat or very likely to get the vaccine was 56% six weeks ago, down from 74% in early April. They also found that only 38% of Black individuals surveyed are likely to get the vaccine. We will need to vaccinate a higher proportion of the population to achieve herd immunity, but the exact number to target is elusive, as described in this excellent report from the Colorado Sun.
Like me, you may have patients in your practice who are reluctant or completely unwilling to receive the vaccine. Dr. Joshua Morganstein, Chair of the APA Committee on Psychiatric Dimensions of Disasters, offers useful advice for discussing vaccination with reluctant patients. Although it is a public health goal to vaccinate the majority of the population, we must be prudent in our approach to this goal. Any heavy-handed policy is likely to backfire given the current political divisions in our country and risks further politicizing the vaccine. Although it is conceivable that eventually some workplaces, such as nursing homes or hospitals, may mandate vaccination for their employees, the legal and ethical implications of such mandates must be considered. Last week, the CDC announced that proof of a negative COVID test or recovery from COVID illness is required for international airline passengers arriving in the US. It is possible that airlines may require proof of vaccination, a so-called “vaccine passport” for air travel, but this is not necessarily going to occur and certainly not until the general public has had a chance to get vaccinated.
One reason some people are refusing to consider the vaccine is the conspiracy theory that Bill Gates has inserted a microchip into the vaccine, which will be used to track the population. A YahooNews/YouGov poll from May 2020 found that 44% of Republicans believe this false claim. I was unable to find a more recent poll, but at least one of my patients continues to fear that this is true. This interview with a social science researcher offers useful advice about how to discuss misinformation with patients, including to not shame the patient either verbally or through your body language, to listen with humility to the patient’s concerns, and to consider this an ongoing conversation over several visits rather than a one-shot (no pun intended) effort to change someone’s mind.
Although it may be tempting to silently or not-so-silently scoff at conspiracy theories, it is more beneficial for us to consider the human tendency to look for patterns or meaning where none exists. This article discusses the evolutionary advantage of slightly suspicious thinking, which both helps us anticipate real threats and makes us vulnerable to conspiracy theories.
Finally, on the topic of vaccines and their funding, this paper describes the effort to create a fentanyl vaccine to protect against overdose. The fentanyl vaccine induces antifentanyl antibodies which bind to any fentanyl that might be used later and prevent it from getting out of the bloodstream and into the brain. The vaccines reduce brain fentanyl levels by 50% to 80%, depending on the dose of fentanyl taken. The fentanyl vaccine effort is funded at a fraction of that for COVID-19, a reflection of stigma by the pharmaceutical industry and the government about the value of investing to save the lives of people addicted to opiates. In the meantime, HHS has made it easier for physicians to prescribe buprenorphine, which isn’t as effective against fentanyl as it is for other opiates but is still saving lives. Any physician with a DEA license may prescribe buprenorphine to up to 30 patients without applying for a separate waiver.
We have two innovative vaccines against COVID-19, and some of us have even received a dose or two, but we are not out of the woods. The more virulent new strain of COVID-19 is present in Colorado and at least 9 other states, and will be the predominant strain by March. I particularly appreciate the boxed comment at the end of this post by my favorite infectious disease blogger. There are many more months to go before it will be safe to relax our diligence. As they say in AA, take it one day at a time.
Stay healthy,
Claire
Colorado Psychiatric Society COVID-19 Resource List
January 20, 2021
|
|
Vaccines - Both CPS and the APA are advocating to ensure our members who need it have access to the vaccines. CPS is in contact with CDPHE and other organizations and is actively monitoring information on the logistics of vaccinations for psychiatrists not affiliated with a facility. If you are category 1B and are having trouble accessing a vaccine, please contact CPS and we will do our best to assist you. See https://covid19.colorado.gov/vaccine for a vaccine distribution flowchart. Additional information at https://covid19.colorado.gov/for-coloradans/vaccine/vaccine-for-coloradans. Also see CMS - Physician Town Hall: COVID-19 Vaccine Update (Webinar, 1 hr 29 mins) (1-14-2021) |
|
APA - Quick Guide to 2021 Office/Outpatient E/M services (99202-99215) Coding Changes (login required). Also see the APA’s Coding and Reimbursement site. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
Thank you to our Platinum Partner for their support
December 23, 2020
Our Balancing Act
By Claire Zilber, MD, DFAPA
CPS President
When I was a child, I was drawn to all manner of activities that involved exercising my balance. One of my favorites was standing on the exact center of a see-saw, one leg on either side of the central pivot point, attempting to keep the see-saw perfectly parallel to the ground. This is the image I hold now as I work to find equilibrium between despair at the ongoing deaths from COVID (320,000 in the US and 4,432 in Colorado as of December 22) plus concern about the long-term neuropsychiatric sequelae of infection, and excited optimism that the Moderna and Pfizer vaccines herald an end to the pandemic.
The neurologic manifestations of COVID are common, varied, and persistent. A small German study found post-mortem evidence that SARS-CoV-2 enters the brain by crossing the neural–mucosal interface in olfactory mucosa. A study of hospitalized COVID-19 patients found that one in seven had neurologic complications, which the study authors believed to be the result of hypoxia. An older study notes cases of encephalitis and Guillain-Barré syndrome, while this recent Spanish case report describes the successful treatment of a 39-year-old man with SARS-CoV-2 encephalitis with interferon and tocilizumab. A study of 29 patients who had recovered from COVID-19 revealed persistent cognitive dysfunction, hypothesized to be due to the inflammatory process. A large analysis of the medical records of 62,354 recovered COVID patients in the US showed that 18% had a psychiatric diagnosis within 90 days of recovery, most often for an anxiety disorder, insomnia or dementia.
Of equal concern are the reports of lingering “brain fog.” This NYT story includes reporting on a nurse practitioner who admits that she’s working in an impaired state. What if she inadvertently harms a patient? What if her licensing board sees this confession? The brain fog is one of the most confusing symptoms among so-called “long-haulers,” those who experience lingering disabilities long after their acute illness has abated. We have all been counting on this nightmare ending, but what about those who develop a chronic illness that persists beyond the pandemic, whose nightmare has no conclusion?
It’s possible that even before we’ve all been vaccinated, we’ll have access to at-home testing to ensure it’s safe to go to work, to school, or on a social visit. The first at-home, 20-minute Coronavirus test received FDA approval last week, and the developer anticipates the availability of three million tests in January 2021. Of course, we’ll need a hundred times that monthly number if we’re going to use frequent testing to open up society before we have all been vaccinated, but more tests are on the way.
Which brings me to another important duty of psychiatrists at this crucial time in the pandemic: we must find ways to fortify our patients’ (and families’ and neighbors’) commitment to pandemic safety while we wait for herd immunity. That workers in ERs and ICUs will be vaccinated by next month protects our healthcare workforce, but doesn’t resolve the problem of maskless people in public. To get people to follow COVID guidelines, it may be helpful to appeal to their care for others. This Harvard study from early in the pandemic found that public health messages focused on protecting others were more likely to inspire compliance with health guidelines than messages focused on the need to protect oneself. If you want to read more about prosocial behaviors, go to The Top 10 Insights from the Science of a Meaningful Life.
I have found nothing motivates my compliance with regulations more than the stories I hear from patients, friends, and the media about the intense suffering of people dying in ICUs, healthcare workers crumbling from exhaustion, families agonizing that they cannot be with their loved ones at the end. Hearing this testimony, I cannot harbor the possibility that my behavior might transmit the virus and disrupt or end another’s life. This JAMA article should be mandatory reading for everyone not on the frontlines. We have included it in our COVID-19 Resources for the Public this week, so feel free to direct people there if they are expressing reluctance to maintain safe behaviors.
Compliance with public health regulations doesn’t mean we are doomed to a gloomy Christmas and New Year devoid of celebrations and diversions. I hope each one of you has a few extra days off in the next couple of weeks, time to slow down the stressful pace, reboot your exercise regimen, connect meaningfully with people you love, and find some frivolous fun.
Do you have a Christmas movie tradition? You can watch the latest blockbuster movies from home. My mother’s childhood family holiday tradition was to travel to New York City to catch a Broadway theatre performance. You can too! Here are some free ones; and here are a collection of Broadway Christmas plays, ballets and concerts. Those of us from the West Coast have other traditions: check out the Christmas concerts and sing-alongs from San Francisco’s Grace Cathedral. Unless you were wealthy enough to fly on the Concorde, never before have you been able to take in a show in New York and join a concert in San Francisco on the same day! A pandemic silver lining, for sure.
If playing games with the clan after opening gifts was your family tradition, that’s still possible. Here are six classic games you can share on Zoom, and another 21 collected here. In case you didn’t know, that activity is called a “covideo party.” Satisfy your word nerd urge with other novel coronavirus neologisms in this amusing article. Go play!
We must remain steadfast in our mask wearing and social distancing until the CDC signals that enough of the population has been vaccinated for us all to be safe. We must balance our optimism and excitement with caution and diligence. Which reminds me of another lesson I have learned from a variety of physical activities. Whether shooting a basketball, serving at tennis, swinging a golf club, or holding an arabesque, the same principle applies: you must maintain your focus and follow through with the physical gesture all the way to the end of the motion in order to achieve success.
Stay healthy,
Claire Zilber, MD, DFAPA
CPS President
Colorado Psychiatric Society COVID-19 Resource List
December 23, 2020
|
|
Reminder: If you should find yourself or know of a physician or physician’s assistant colleague that needs support for the stresses of the COVID-19 crisis, and caring for those afflicted, please reach out to the COVID-19 Care Line for Physicians at 720-810-9131. |
|
APA - Resource Document - How Psychiatrists Can Talk to Patients and Families About Race and Racism - resource developed by the APA Council on Children, Adolescents, and Their Families in consultation with the APA Presidential Task Force to Address Structural Racism Throughout Psychiatry (11-20) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
December 9, 2020
Lighting the Candles of Resilience
By Claire Zilber, MD, DFAPA
CPS President
Chanukah begins Thursday at sundown, celebrating a miracle. A vial of sacred oil, only enough to keep the everlasting light illuminated for one night, lasted eight nights, long enough for the community to acquire a fresh supply. This year, that story feels particularly relevant. We know relief in the form of a vaccine is on its way to us, but we are not the first in line for it, and it will be a while before our communities are safe. As we witnessed over Thanksgiving, many people are so exhausted by the pandemic restrictions, so in need of connection, that they threw caution to the wind. The case rates reflect the result, yet the anticipated spike from Thanksgiving gatherings won’t show up until later this week. We must double down on safety over the winter holidays, or we will have a nightmarish January. What oil can we find to sustain our hope and renew our diligence? After reviewing some information about the exhaustion and depletion that are real for all of us, I’ll bring you some good news and suggestions.
Holidays are hard in a pandemic, especially in the tenth month of social restrictions. Our colleague and former CPS President Peter Mayerson coined the term “sequesteritis.” I want to see my friends’ unmasked smiles. I yearn to give them hugs. I long to visit my mother. I’m only one of 7.8 billion people on this planet who share these feelings. Our Brains Explain the Season’s Sadness reports on why we all are so depleted. According to the neuroscientist interviewed for the story, our prefrontal cortex is working overtime to keep an eye out for all the threats we face. Remaining vigilant about the coronavirus, civil unrest, political turmoil, job insecurity, the wellbeing and education of our children, wildfires, hurricanes, and separation from family takes a lot of energy. Add to that the extra focus required to work and socialize on a screen, or to work in PPE, and you’ve got one very tired brain. Although the phrase “deaths of despair” predates the pandemic, it is especially fitting now as preliminary data suggests deaths from drug overdoses have doubled.
Like a lotus emerging from mud, there are glimmers of good news arising from the nightmare of the pandemic. Researchers observe a decline in youth vaping in the pandemic, and this commentary includes suggestions for ways to intervene to maintain this trend after pandemic restrictions are lifted. Since youth vaping is linked to marijuana use, a reduction in the former may have a significant impact on the pathway to addiction.
Another measure of good news oil is that the pandemic has increased our access to online material that we can use in our work. Take, for example, this stigma-busting video discussion between two women in the publishing industry, one with dyslexia and the other with bipolar disorder. It includes reflection on how the pandemic has added further complexity to managing their neurodiversities, as well as valuable information about combatting shame, and advice to managers who supervise people with neurodiverse qualities. We have dropped this into the COVID-19 Resources for the Public page on the CPS website, so you can share it with your patients.
One of the conversation starters at CPS' Monday evening cranberry-margarita-infused Winter Party was to identify a way each of us has grown during the pandemic. Albert Einstein wrote that “Adversity introduces a man to himself.” The pandemic provides an opportunity to dig more deeply into ourselves for the strength to endure; we will be changed. As psychiatrists, we have the privilege to help others who might otherwise break under this pressure, help them find their resilience and emerge from the storm. In my work these last few months, I find that empathetic humor is especially helpful in those moments when someone is describing their latest personal calamity piled upon this collective disaster. Something about the release of laughter eases the tension on the soul, and we find we can bend a little further after all. In that spirit, I was delighted to read JAMA’s best of 2020 Graphic Medicine. If you don’t have time to click on all the links inside that review, here are two highlights. This comic by Gemma Correll, Creativity in Captivity, pokes fun at what she plans to do during the shelter-in-place order vs. what she actually does. Another gem in the JAMA review was the revelation that there’s an annual conference on graphic medicine, and that they have created a free, monthly virtual meet-up during the pandemic called Drawing Together. Free art therapy for us!
Good news, humor and art therapy are some of the extra oil we need to keep our lanterns lit, to help us find the will to stay safe for a few more months as we wait our turn for the vaccine and then wait a little longer for enough of the population to be immunized so that we all can be safe. The CDC’s recent revision of quarantine guidelines applies a scientific lens to choosing a length of quarantine based on risk. I find the graph especially helpful in illuminating the difference between 7, 10 and 14 days of quarantine, and the table below it clarifies how adding a negative PCR or antigen test may increase confidence about reducing quarantine from 14 to 10 days. I also was reassured to see what precautions epidemiologists are taking in their personal lives; apparently, that I do not place my mail in quarantine does not make me a daredevil. Whew! When a physician friend told me that he is only doing the top four activities on the chart, I felt a competitive zing because I’m only doing the top three. Hey, if friendly competition is what it takes to keep me safe, I’m all in. In the end, I’d rather have sequesteritis than coronavirus.
Although I didn’t set out to include eight positive links in this letter, to correspond to the eight nights of Chanukah, it worked out that way. There is your oil. Now light your candles and those of your patients so that we all retain the fortitude to manage our behavior, reduce our risk of acquiring and transmitting the virus, and further develop our capacities for endurance and resilience.
Stay healthy,
Claire
Colorado Psychiatric Society COVID-19 Resource List
December 9, 2020
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Also see NYT - I Achieved My Wildest Dreams. Then Depression Hit (5 min 30 sec video) I’d spent my life training for the Olympics, but I wasn’t prepared for what came next - Elite athletes and coaches should be trained to monitor mental health as much as physical injuries, argues Alexi Pappas, an Olympic runner who shares her own struggles with depression in a new video (12-7-20) |
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
|
|
November 25, 2020
Suffering and Hope: The Pandemic Thanks Giving
By Claire Zilber, MD, DFAPA
CPS President
Psychiatrists are a strange and wonderful breed. Whether through training or natural inclination, we develop our unique superpower: the capacity to hold the suffering of others while radiating hope. As we descend into the pandemic winter, the dialectic of suffering and hope will persist.
Let’s begin by witnessing the suffering. The US has had over 12,422,000 COVID cases, and 257,700 deaths. Colorado has had over 203,600 cases and 2,820 deaths. Mesa County, a model of public health preparedness early in the pandemic, has run out of hospital beds, and hospitals across the state are struggling with ICU capacity, non-ICU capacity and staff capacity. Frontline healthcare workers are under severe strain, as are just about everyone else.
According to the Pan-American Health Organization, only 2 of the 29 countries in the Americas have an adequately funded mental health plan for the pandemic. Their report doesn’t name names, but I’ll venture that the US is not one of the lucky two. A recently published survey of mental health across the United States, Canada and Europe showed increased levels of anxiety and depression, but the data was collected in March and April, so it doesn’t inform us about the current state of population mental health. We know that pediatric ER visits for emotional distress rose after March 2020, as described in this CDC report. What is not yet captured in published data but is plainly evident is the further increase in distress in the last two months. The election set us on edge. Everyone has grown weary of pandemic precautions. We tire from lack of a good vacation, from missing distant family, from deprivation of singular pleasures like fine dining and heartfelt hugs from friends. Psychiatrists don’t need data to know this because we hear it first hand: our patients are more distressed and they have exhausted their coping reserve.
Without a doubt, Colorado does not have an adequately funded mental health system. Mental Health America ranks our state 33rd based on prevalence of mental illness and low access to treatment. We have the seventh highest suicide rate of all the states, according to the CDC. Governor Polis has taken steps to improve mental health and substance abuse treatment services in the state, and you can learn much more about those efforts from the Putting People First report. Governor Polis established the Behavioral Health Task Force (BHTF) to reimagine the behavioral health system in Colorado. CPS member Dr. C. Neill Epperson served on the main BHTF and the following CPS members served on subcommittees of the Task Force: Drs. Richard Martinez, Alexis Giese, Sasha Rai, and Kimberly Nordstrom. The Blueprint for Reform has 3 phases. The first step is creating a Behavioral Health Administration to coordinate a centralized response to our mental health crisis. The second step will be increasing access to services for crisis support and ongoing treatment. The final phase will focus on assessing and implementing remaining recommendations. This is vital work, but it is also woefully overdue and of no help to the many people who are suffering right now.
How do we infuse hope into our pandemic-weary patients and selves given our resource-poor mental health environment? Christina Figueres suggests relentless optimism. In her TED Talk, she discusses the optimism required to achieve a global accord on combatting climate change, but her points apply equally well to every other pressing national and global issue, including the pandemic. She defines optimism as a conglomerate of courage, hope, trust and solidarity. Is it worth 15 minutes of your time to watch this TED Talk? Only if you want to be uplifted by admiration and inspired to your own internal shift away from cynicism.
Relentless optimism reminds me of the DBT skill of radical acceptance, which in turn inspires “radical gratitude” about Operation Warp Speed. Despite the many blunders and general incompetency of our federal response to the pandemic, Operation Warp Speed appears to have yielded impressive results, for which we may all be unreservedly grateful. This Lancet article expresses optimism and simultaneous reservation about the three vaccine announcements (including Russia’s) in the last two weeks. The manufacture and distribution of vaccines in an equitable manner both nationally and globally raises difficult logistical and ethical problems. But how exciting to have arrived at the opportunity to address these problems!
This CDC communication inspires optimism that they might counter vaccine skepticism with reassurance about safety and efficacy monitoring, and the extent of CDC coordination with other government agencies. Further hope rests on the knowledge that many other vaccines as well as alternate, creative medical approaches are under development, such as inhaled interferon to protect pulmonary tissues from infection.
Last weekend, the FDA issued an emergency use authorization (EUA) for a combination monoclonal antibody treatment, casirivimab plus imdevimab, for patients with mild-to-moderate COVID-19 who are at high risk for developing severe disease (for example, adults aged 65 and older). This is the same treatment given to President Trump. The EUA was issued based on findings from a randomized placebo-controlled trial of 800 outpatients with mild-to-moderate COVID-19. Patients who received the active treatment were less likely to be hospitalized or visit the emergency department within 28 days.
Late last week the FDA also issued an EUA for the combination of baricitinib (an oral janus kinase inhibitor) and remdesivir to treat hospitalized COVID-19 patients who require supplemental oxygen, invasive mechanical ventilation, or extracorporeal membrane oxygenation. In a randomized placebo-controlled trial of 1000 patients, those given remdesivir plus baricitinib, versus remdesivir plus placebo, had a shorter time to recovery and were less likely to die or need mechanical ventilation within 29 days of treatment.
In research news that may be especially exciting to psychiatrists, two weeks ago a randomized placebo-controlled trial found that the antidepressant fluvoxamine may have a role in treating novel coronavirus infection. In addition to being an SSRI, fluvoxamine is also a strong S1R agonist. The S1R is an endoplasmic reticulum chaperone protein with various cellular functions, including regulation of cytokine production. Previous studies have shown that fluvoxamine reduced damaging aspects of the inflammatory response during sepsis through the S1R-IRE1 pathway. In this preliminary study of 152 adult outpatients with symptomatic COVID-19, patients treated with fluvoxamine (100mg TID) had a lower likelihood of clinical deterioration over 15 days. Psychiatrists may actually be able to prescribe something within our scope of practice to actively treat symptomatic patients!
Although Christina Figueres doesn’t include gratitude in her list of optimism-inducing traits, I believe that gratitude is a powerful prompt to a more positive mindset. By focusing on what is good, our outlook about our circumstances shifts. I am grateful for all I am learning with my patients. As we struggle together to navigate and endure the many difficulties encountered this year, I strengthen and broaden my own coping skills. I’m grateful to have a purposeful focus each day, whether that’s direct patient care, practice administration, continuing education, teaching, or CPS activities. I am grateful for technology, which has helped us adapt in all our work and social environments. Nine months ago, I never imagined I would be facile with telehealth, teaching by Zoom, electronic prescribing, electronic lab orders, even electronic file sharing through the telehealth portal! I am grateful for all the hospital workers who are putting in extra hours, isolating from their families, risking their lives, stressed to the max yet still trying to provide comfort to dying patients. And I am grateful for all the other essential workers who put themselves at risk to keep society somewhat functional.
Suffering, hope, gratitude. We cannot transmit hope to our patients without first witnessing their suffering. We cannot bear to absorb their suffering without holding on to hope. We cannot reach for hope without awareness of what remains in the world that is good, and give thanks for all of it.
Stay healthy,
Claire
(Gratitude to Dr. Jenny Kennedy for bringing to my attention the TED talk on optimism.)
|
Interested in learning about the outcomes of the Governor’s Behavioral Health Task Force and potential legislation in the 2021 session? The event features CPS members C. Neill Epperson, MD and Elizabeth Lowdermilk, MD, along with CDHS Executive Director Michelle Barnes and others. This activity has been approved for AMA PRA Category 1 Credit NOTE: You do NOT need to be a CMS member to attend this event. if you do not have a CMS member number or do not know your CMS member number, you can write n/a or enter any number when requested in the registration form |
Colorado Psychiatric Society COVID-19 Resource List
November 25, 2020
|
|
Register for all 4 upcoming CPS events - The pandemic may hinder us from gathering in person, but CPS is here to ensure you have ample opportunity to stay connected to friends and colleagues. Event details at https://www.coloradopsychiatric.org/events. |
|
NYT - How to Have a Fully Remote Family Thanksgiving - Skipping travel this year to stop the spread of Covid-19? Here’s how to digitally reimagine the holiday, from meal prep to after-dinner activities (11-18-20) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
|
|
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
November 11, 2020
Inpatient Psychiatry in the Pandemic
By Claire Zilber, MD, DFAPA
CPS President
For many of us, our first exposure to the field of psychiatry was as a student on an inpatient ward. In college, a course on Abnormal Psychology included a field trip to the Philadelphia State Hospital where each student was paired with a patient. I was assigned to a man with Tourette’s syndrome, who shouted obscenities while pacing the halls and gesticulating. I imagine how dangerous life would have been for him in public, where people would misunderstand his illness as aggression; however, at the time, he alarmed me so much I could barely conduct the interview. An inpatient unit is simultaneously a safe haven and a scary place, and the pandemic has amplified this dichotomy. This week I’ve explored the risks particular to inpatient psychiatric settings, the guidance issued to help mitigate those risks, some ethical quandaries that have emerged, and several creative solutions.
As if obstacles to inpatient admission weren’t already extensive, including insurance barriers, bed shortages, stigma, and past traumatic experiences with treatment, now patients may fear presenting to the hospital because of COVID. Indeed, this report from February about an outbreak in a psychiatric hospital in South Korea, which led to over 100 infected patients and 17 deaths, reinforces beliefs that the hospital is unsafe. Lest we think such carelessness couldn’t happen here, this September 29 article from The Gazette reports on the closing of a psychiatric hospital in Johnstown (just east of Loveland) because of inadequate pandemic precautions as well as allegations of patient abuse.
Unlike medical and surgical units, psychiatric units are organized around the therapeutic milieu, based on the concept that interactions among patients as well as with staff have therapeutic value. How can we maintain a group milieu while isolating potentially infectious patients? Some direction has been provided by our government. For example, this SAMHSA guidance, issued in May, considers ways to reduce morbidity and mortality by mitigating risks for patients and staff while preserving the functioning of the healthcare system. Updated October 13, here is the link to the APA’s practice guide for COVID-19. Scroll down to the heading on inpatient psychiatry. These resources relate to a March 18 guidance issued by CMS (Centers for Medicare & Medicaid Services) about tiers of care, which triggered APA’s statement that ECT should be considered an essential procedure, not an elective procedure that could be postponed during a lockdown.
More substantial guidelines have been offered by our colleagues. This July 2020 literature review about psychiatric care in the US during the pandemic addresses all locations of psychiatric treatment (ie: outpatient, emergency rooms, C/L, and inpatient). Scroll down to section 3.3 to read their findings about inpatient psychiatry, and then move on to section 4, which includes a consideration of the ethical implications of admitting patients to an inpatient unit, which some have compared to a nursing home in terms of exposure risk. Informed consent about this risk is necessary, but may be difficult to obtain from a psychotic patient. This excellent double case report highlights ethical and logistical considerations when caring for older adults on inpatient psychiatric units. This paper from the Journal of Medical Ethics also uses a case study to elucidate ethical dilemmas and policy recommendations for when patients refuse COVID-19 testing and won’t comply with quarantine or social distancing on psychiatric inpatient units.
A variety of adaptations have been adopted across the country. The University of Rochester created a COVID-19-positive psychiatric unit so that inpatients can benefit from the milieu and group support while also receiving expert medical care. In Colorado, the predominant model (based on information from Denver Health and Porter Hospital) is to hospitalize COVID-positive psychiatric patients on the medical service and support those patients with telepsychiatry from the C/L team.
Telepsychiatry is not being used on the inpatient service at Denver Health. Patients are tested prior to admission, and only those who test negative are admitted to the psychiatry unit. Staff and patients are screened for symptoms daily, social distancing is enforced as much as possible, mask wearing is encouraged, and the unit is frequently sanitized. Groups and other therapeutic programs are being continued. Initially quiet, the inpatient units at Denver Health have been busy since September, which likely reflects the “mental health wave” of the epidemic we’ve been anticipating. Staff have remained healthy, with only four positive tests among the inpatient and ER teams, all of whom recovered quickly. Staff burnout is a big concern, as is how to manage patients who refuse COVID testing (go back to the Journal of Medical Ethics case study to read the discussion about balancing a patient’s right to auonomy against the public health imperative to not place other patients and an entire staff at risk).Staff burnout and maintaining inadequate staffing are real problems. The compelling part of this article addresses how longstanding problems with understaffing and inadequate inpatient beds, which leads to long stays in non-therapeutic emergency departments, has been exacerbated by the pandemic. One psychiatrist has accelerated his pre-pandemic project to create truly therapeutic spaces for psychotic or suicidal patients in emergency departments, with the goal of being able to send 75-80% of patients home without inpatient admission. Similarly, this report from a London hospital asserts that the kinds of adaptations we see happening now may lead to positive changes in inpatient units that will persist beyond the pandemic. For example, they instituted point-of-care testing for clozapine levels, which expedited dose titration; enhanced videoconferencing connections with community agencies to facilitate a smooth and efficient discharge plan; and even used telehealth to meet with patients’ family members during rounds.
Inpatient psychiatric services are a crucial component of mental health treatment, and will continue to be necessary throughout the pandemic and its aftermath. While the challenges COVID-19 has brought to inpatient psychiatry are formidable, the solutions emerging from this crisis reveal the creativity and adaptability of our colleagues. We don’t have all the answers, but at least we’re identifying important questions to help respond to the needs of acutely psychotic or suicidal patients while containing the risk of infection as much as possible.
I am grateful to Drs. Steve Mayes, Beth Cookson and Christian Thurstone for their valuable contributions.
Colorado Psychiatric Society COVID-19 Resource List
November 11, 2020
Updates |
|
9News - Here are the Colorado counties that are moving to tighter COVID-19 restrictions - A list of Colorado counties that have recently tightened restrictions due to an uptick in COVID-19 cases. Includes information on Denver’s Home by 10 curfew (updated 11-9-20). Also see the Colorado County COVID-19 dial dashboard (updated daily) |
|
CO HCPF - Register for the Telemedicine Stakeholders Engagement Meeting - Thursday, November 12, 2020 4:00 PM MST - 5:00 PM MST - The Department of Health Care Policy and Financing is continuing its consideration of telemedicine policies and their effects on access, quality of care, budget, and provider and member experiences. Their goal is to ensure that members have access to quality telemedicine services while managing their fiscal responsibilities. They have been assessing and developing policy around telemedicine. Proposed policy will be shared and feedback requested. |
|
APA - Register for the APA Town Hall on Structural Racism, Part 3: The Trauma of Structural Racism and its Transmission Across Generations - Monday, November 16 | 6-7:30 MT (8:00 - 9:30 p.m. ET) - Disparities in mental health for people of color remain pervasive and persist across generations. There is a growing consensus that structural and interpersonal racial discrimination fundamentally impact mental health in communities of color. The persistent stress of experiencing discrimination has an impact across generations, and the degree to which the health consequences of racism and bigotry can be passed down from one generation to the next is an important avenue of exploration. This town hall will delve into this issue. Have a question you would like the panel to address? Submit your question at this link. |
|
APA - Register Here for an Update on 2021 Changes to Billing and Documentation for Outpatient E/M Services - Tuesday, November 17, 6pm MT (8 pm ET) - Join this webinar to learn about the changes to billing and documentation for Outpatient E/M services that will take effect on January 1, 2021. The webinar will include how to select the appropriate CPT code based on medical decision making or time, a review of the necessary documentation, and a Q&A portion with APA’s CPT coding and documentation experts. Also see Bump in Medicare Values for E/M Codes Could Increase Psychiatrist Payment (8-31-20) and AMA - E/M office-visit changes on track for 2021: What doctors must know (8-5-20) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
|
|
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
October 28, 2020
More Tricks than Treats: Psychiatric Sequela of the Pandemic
October 28, 2020
All but one of my patients on Monday was dispirited about making it through this winter. Worn down by almost eight months of health anxiety, social restrictions, inability to visit far-flung relatives, and political angst, the frigid conditions early in the week seemed to knock the wind out of almost everyone. The alarming surge in cases in Colorado, with over 2100 new cases reported on Sunday and a new case rate of 24.3 per 100K residents, is a great concern, dwarfed only by the reality that every single one of our neighboring states is faring even worse, according to Johns Hopkins University. In this letter, I offer an update about psychiatric sequelae of COVID-19 infection itself, managing chronic mental illness during this pandemic, and coping with depression. Lest this leave you hollowed out in despair, I promise levity at the end.
Psychiatric Conditions Associated with COVID-19
There appear to be several different biological pathways to psychiatric syndromes as a result of COVID infection. Acute syndromes include delirium, and symptoms related to acute stroke caused by the vascular manifestations of infection. Later psychiatric symptoms may be the result of immunologic responses to infection, and perhaps from the ongoing presence of the virus within the CNS (within endothelial cells, macrophages or monocytes). There is so much more to learn about this virus. To the extent that the CNS may serve as a reservoir for infection, as it does for HIV, we may find long-term psychiatric sequelae emerging months or years after initial infection. For now, we must content ourselves with hypotheses about mechanisms of illness, and small studies, which were recently reviewed in this paper. The reviewers found only two studies of psychiatric conditions in patients with COVID-19, which showed high rates of PTSD and depression in those patients. The remaining studies examined the indirect effect of the pandemic on wellbeing among patients with chronical mental illness (CMI), the general public, and the healthcare workforce.
Coping with CMI in the Pandemic
For patients with CMI, the pandemic has added new burdens to an already overburdened and under-resourced population. With most outpatient clinics operating via telemedicine, patients without reliable access to the internet or whose paranoia interferes with their willingness to use telehealth are less able to engage in treatment. As discussed in this Kaiser Health News article, acute treatment settings like ERs, inpatient units, detox centers, and residential treatment facilities are now even more difficult to get into than usual because beds have been reduced to keep patients and staff safe during the pandemic. Furthermore, patients with CMI have more medical comorbidities than the average person, yet they have less access to medical care, a problem likely to be exacerbated in the pandemic. The Canadian authors of this article suggest mitigation strategies that are equally applicable in the US, such as increasing access to low-cost technology so that patients can access telehealth regardless of their economic means, as well as bolstering resources to support collaboration between primary care and psychiatry. Another unique intersection between COVID-19 and patients with psychosis is highlighted by this case report of a patient on clozapine who was hospitalized for COVID-19 in the UK. The patient developed toxic levels of clozapine, presumably because cytokine release associated with COVID-19 infection downregulates CYP 1A2, thereby slowing the metabolism of clozapine.
Coping with Depression in the Pandemic
By now, it has been well documented that rates of depression have soared as a result of pandemic related stresses including grief over the deaths of loved ones, hardship because of loss of employment, job/food/housing insecurity, isolation because of physical distancing restrictions, and a surge in domestic violence. Because the pandemic has required massive adaptation for almost all of us, any form of psychotherapy focused on navigating the many changes and stressors in our environments is key to effective treatment. Some authors advocate specifically for Interpersonal Psychotherapy for patients and families, while others recommend Cognitive Behavior Therapy for frontline workers. The impact of grief on family members of COVID-19 victims and healthcare professionals on the frontlines who are experiencing multiple deaths on their watch is of particular concern. We know from previous research that sudden and traumatic loss, as well as multiple sequential losses, are more likely to result in prolonged grief disorder. This article addresses the potential scope of grief as a result of the pandemic, and offers a public health/community strategy for managing a grieving population, including more training for primary care providers and referral to mental health for the more complicated cases, such as those involving psychosis or suicidal ideation. In this PsychNews story on suicide prevention strategies for the pandemic, I followed the link to a free training on CALM: Counseling on Access to Lethal Means. It takes around two hours to complete the training. While much of the information is familiar to psychiatrists, this may be an important time for us to refresh our suicide prevention counseling skills. There are additional articles in this week’s Resources for Providers about depression and suicide in the pandemic.
Enough Tricks, Time for Treats
I admit to my own trepidation last weekend: how will I be able to help all my patients keep their heads above water if I don’t stay well myself? I was bolstered by this NYT story on What Scandinavians Can Teach Us About Embracing Winter. We include this in our Resources for the Public page, so please remember to direct your patients and others to that page. It helped me reframe my dread by reminding me of all the treats that come with cold weather: hot beverages, cozy sweaters, improved sleep on crisp nights, opportunities to invent new favorite soups, “owning the park” when I walk my dog on mornings too cold for others to venture out, snowshoe day-trips with friends, and so much more. In addition to leaning on old favorites, I intend to create new traditions. For example, with the Blue Moon on Halloween, I plan to drink a Blue Moon beer, listen to all the different covers of Rodgers and Hart’s Blue Moon, and gaze at our beautiful satellite. For those of you adapting the holiday for children, I appreciate the tips at the end of the CDC’s Guidance for Halloween, especially the inspiration to hold a treasure hunt at home in lieu of trick-or-treating in the neighborhood. I love treasure hunts! If all else fails, and the winter doldrums suck the life out of you, try Yoga for When You Feel Dead Inside.
Colorado Psychiatric Society COVID-19 Resource List
October 28, 2020
Updates |
|
COVID-19 Exposure Notifications have started in Colorado! You can now activate this service to protect your community while maintaining your privacy. CO Exposure Notifications can quickly and anonymously notify you if you’ve likely been exposed, allowing you to reduce risk for your loved ones, seek timely medical attention, and stay home. Find out more at addyourphone.com. |
|
Mayor Michael Hancock announced two additional public health orders in Denver. Also see yesterday’s update - State Moves Denver Back to Level 3 Restrictions - CDPHE has moved the City and County of Denver, among other counties, to the more restrictive Safer at Home Dial Level 3 (10-27-20) |
|
CPR - New Health Order Limits Personal Gatherings To 10 People From No More Than 2 Households In Most Counties (10-23-20). Also see amendment to the health order (download) (10-23-20) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
October 14, 2020
Ethical Dilemmas in the Pandemic
The pandemic has prompted unprecedented changes in healthcare, including psychiatric practice. Telemedicine is suddenly mainstream and is changing norms before we can consider their ethical implications. Discussions about rationing care, a very taboo notion in the US, were widespread in the spring when hospital beds and ventilators were scarce in Italy, Spain, England, New York, and other hotspots. Decision-making algorithms for access to ICU beds and ventilators and for administration of vaccines are covered in the medical literature and lay media. Concerns about the ethical implications of rushing a vaccine through the regulatory process have become a touchy political issue, and medical editors are issuing political opinions in advance of the presidential election. This is more fodder for ethical analysis than can be managed in this space, so I will focus on three areas most relevant to psychiatrists: boundaries within telehealth, C/L psychiatry and COVID-19 ethics, and an ethical approach to public health policy.
In May 2020, the APA conducted a member survey about their use of telehealth before and after the public health emergency caused by SARS CoV-2. Whereas before the pandemic 64% of respondents used no telehealth in any of their patient encounters, a mere two months later 85% were using telehealth for 76-100% of their clinical work. Initially, we were mostly focused on getting the technology to work for us and our patients, paying attention to only the most obvious ethical issues, like privacy and confidentiality in clinician and patient environments. The APA’s Best Practices in Videoconferencing-Based Telemental Health states, “During a telemental health session, both locations shall be considered a patient examination room regardless of a room’s intended use.” We fretted about how to ensure the patient’s room is private if we can’t see the entire space. Eventually, other concerns surfaced, like hidden obstacles to confidentiality in the form of eavesdropping or recording devices. If the psychiatrist or the patient has an Alexa or Echo device within earshot, might it start recording or even speaking in response to what it hears? Might the patient intentionally record the session without the psychiatrist’s knowledge or consent? Might the psychiatrist do so without the patient’s consent?
Telepsychiatry has provoked a loosening of boundaries. A previous article on boundaries written in April feels quaint six months later. Then, it felt awkward that patients could see one wall of my home. Now, many of them ask to see my dog if they hear him bark or squeak a toy. To deny that request would seem cruelly withholding. Only recently have I considered that my dog could be in a different room when I have patient appointments, reducing the temptation to cross this boundary. This opinion piece by Lori Gottlieb, author of Maybe You Should Talk to Someone, reveals several ways in which the loosening of boundaries because of seeing patients in their homes (or cars, backyards, front porches, sidewalks… ) enhances the therapy. On the other hand, I’m disconcerted that she admits to downgrading her wardrobe. I believe it is more professional and respectful to dress as we would if we were in our offices.
Just as outpatient psychiatrists are faced with a variety of new ethical dilemmas, C/L psychiatrists are encountering new challenges, too. When should they see a patient in person, using up precious PPE, and when is it better to do an evaluation via telehealth? Is the decision to use telehealth a convenient rationalization for reducing personal risk of exposure, or a sound policy? This article from UCLA strongly argues the latter, not just for psychiatrists but for all medical personnel who don’t absolutely need to touch the patient. In addition to adapting their consultations to include telehealth when appropriate, C/L psychiatrists may encounter new kinds of consult requests, such as evaluating whether a patient has capacity to request to leave the hospital AMA during the pandemic, or assessing the patient who wants to change their status to DNR in order to conserve resources for others. Johns Hopkins has published an excellent resource, Capacity Assessments During the COVID-19 Pandemic, to help clinicians navigate these unique situations.
In addition to new ethical dilemmas for outpatient and C/L psychiatrists, we may also focus on the ethics of public policy decisions during the pandemic. We are experts on cognition and communication, and can help shift the conversation about personal responsibility for public health (ie: wearing masks and conforming to physical distancing guidelines) when we notice and correct bias in messaging. This paper, Cognitive Bias and Public Health Policy During the Pandemic, identifies four types of bias evident in the public narrative that compromise public safety. Another article focuses on the virtues of compassion, solidarity and justice as important guides to public policy in the pandemic. When we incorporate these themes into our discussions with reluctant patients, workplace administrators, and policy makers, we advance the conversation along ethical lines.
Perhaps the most distressing ethical problem highlighted by the pandemic is the absence of justice (equal access to treatment for all) in US healthcare. While the President is able to receive an experimental monoclonal antibody in Phase II trials, 44 million Americans are without health insurance. Much has been written about disparities in health outcomes during the pandemic; this summary from SAMHSA is a good place to start if you want to delve more deeply into the intersections between race, behavioral health and COVID-19.
In closing, this letter identifies several ethical dilemmas uncovered by or created by our responses to the pandemic. There are many more. I will devote a future letter to inpatient psychiatry during the pandemic, including ethical issues encountered in that setting. If you have other pandemic-specific ethical questions, please contact me through [email protected] and I will endeavor to address them in later letters.
Stay healthy,
Claire
Claire Zilber, MD, DFAPA
CPS President
Colorado Psychiatric Society COVID-19 Resource List
October 14, 2020
Updates |
|
Application can be made here: Provider Relief Fund Application and Attestation Portal. Deadline: November 6, 2020 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
|
|
September 30, 2020
ON HOPE
Claire Zilber, MD, DFAPA
September 30, 2020
“Hope is being able to see that there is light despite all of the darkness.” Desmond Tutu
As the Jewish New Year starts and the secular year crosses the threshold into its last quarter, the world feels desolate. We’re ten months into a global pandemic with no end in sight, which has sickened more than 33 million and killed over one million people globally, with over 7 million cases in the US and 205,676 deaths (from Johns Hopkins). Conspiracy theories complicate responses to the pandemic, as personal participation in precautions and attitudes towards accepting a vaccine vary depending on one’s beliefs. Police killings disproportionately affect people of color, provoking months of protests, which in turn have sometimes led to violent clashes with counter-protesters. Economic distress because of pandemic shutdowns has led to food and housing insecurity for millions of Americans. Wildfires have scorched over five million acres across the West, a fairly abstract number that this article attempts to contextualize. Ruth Bader Ginsberg’s death has unleashed political shenanigans which are deepening our national strife, and the upcoming election has everyone on edge regardless of their political affiliation. This is a lot to hold as we go about our work, trying to help people regain and sustain mental health. I have labored in the last two weeks to reframe my despair so I can be useful to others. I look both to the past and the future to bolster my hope, and eventually end up in the present.
On the Sunday evening following Ruth Bader Ginsberg’s death, a conversation with my father-in-law planted the seed of perspective. He reminded me that things looked grim throughout much of World War II until Hitler’s army encountered the Russian winter. An unforeseen ally in the war, it turned the tide. I have been trying to imagine the thoughts and feelings of the inhabitants of France, Poland, Greece, England, and other European countries that were either occupied or imperiled by fascist forces. However menacing we feel our situation may be, the circumstances in WWII were even more dire. Yet, in the end the Allies prevailed, Europe was rebuilt, and the European Union eventually emerged, joining former enemies as partners.
Karl Menninger’s 1959 lecture to the APA Assembly addresses hope in the context of healing. He, too, goes back to WWII, to the Buchenwald concentration camp, to find an example of hope against all odds being marshalled by the physicians who were also prisoners to sustain themselves and help their fellow inmates. This eloquent lecture places hope squarely at the center of psychiatric education and practice.
Just as the world didn’t know what would happen next in the waning months of 1942, we don’t know what will happen as 2020 winds down and hands over this turmoil to 2021. Cringing, we may ask, “Can it get any worse?” I do my best to avoid that thought path, which can lead to apocalyptic fears. Instead, I focus on the signs pointing toward hope. Let’s begin with Anthony Fauci, who offered two reasons for hope earlier this month. He noted that there is a significant response in infection rates when communities choose to adhere to public health recommendations, indicating that we can control the pandemic through our collective action. He also noted that three vaccines are in phase three trials. It’s worth clicking on this link just to see Dr. Fauci’s smile, which reliably triggers a small relaxation response in my nervous system.
Additional reasons for optimism include a spate of recent papers demonstrating the efficacy of corticosteroids in critically ill patients with COVID-19. There is now enough evidence of utility for this readily available, inexpensive medication for it to be a first line treatment for severely ill patients. This JAMA editorial offers a nice mini-review of the literature. Even better news is that two saliva tests for SARS-CoV2 received FDA approval last month. They need to be scaled up, but eventually we could end up where Dr. Paul Sax, my favorite Infectious Disease blogger, suggested we go way back in July, with at-home rapid testing. Even without a vaccine, we could be back in the office face-to-face with our patients if everyone was doing daily home testing. Finally, the Chief of the World Health Organization expresses optimism that the pandemic will end in less than two years, which will make it shorter in duration than the 1918 influenza pandemic. He says our advanced technology will allow us to respond more quickly and effectively than a century ago.
Another reason we may progress quickly is the fact that so many of the world’s scientists are all working on the same problem at the same time. This spurs innovation. For example, a research team at UC San Diego is adapting nanosponge technology, originally developed to treat bacterial pneumonia, to protect pulmonary tissue from the coronavirus. This delightfully optimistic editorial from the Canadian Family Physician projects that, having worked collaboratively to address the pandemic, the world’s scientists will learn how to come together to address other global crises such as climate change and poverty.
In addition to scientific advances in response to the current swirl of crises, we may see changes at the individual level. This military psychologist writes about post-traumatic growth, a phenomenon seen in combat-exposed soldiers. He describes a potential for many of us to go beyond resilience to personal improvement, and says that skills to foster a positive outlook, spirituality, active coping, self-efficacy, meaning-making, and acceptance of limits and circumstances can all be taught. Psychiatrists are in a prime position to teach these skills to our patients. There is a wealth of articles about adaptation and staying positive, such as this one. Indeed, you will find many others on the CPS webpage of resources for the public.
The current state of affairs is beyond stressful. Our lives are disrupted and we feel uneasy. Yet these are the very conditions that can bring about innovations and cause transformations in individuals, communities, and societies. Who would have imagined that we would transition so quickly to telehealth? This is a change in healthcare practice that will not disappear after the pandemic ends. Who would have predicted that TaNehisi Coates’ Between the World and Me would be on the NYT Bestseller list for over 100 weeks? This reflects a society-wide interest in understanding and resolving racism that will not revert. Seven months ago, I would never have believed that some of my more reluctant patients would be doubling down on their self-care practices, but they have demonstrated to themselves that meditation, exercise, gratitude lists, or whatever works for them is actually worth the effort. They cannot unlearn these skills. We have been changed, as a society, as a profession, and as individuals.
Colorado Psychiatric Society COVID-19 Resource List
September 30, 2020
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
September 16, 2020
Physician Mental Health During COVID-19: A Call to Action
I imagine that all healthcare professionals (HCPs) are experiencing a surge in stress during the COVID-19 pandemic. We all need resources to take care of ourselves so we can perform well in our care of patients. Physicians as a group are self-sacrificing, dedicated to helping others, and loathe to ask for help or show signs of weakness. Medical training amplifies all these characteristics. It is a painful irony that, at this time of surging HCP distress, the peer assistance organization to which we have turned for 34 years for confidential assessment and treatment monitoring is under serious threat. In this letter I will discuss HCP distress during the pandemic, consider how moral injury has been amplified by the pandemic, introduce the threat to CPHP as a unique cause of moral injury to Colorado physicians and physician assistants, and present potential solutions.
As early as March of this year we were seeing reports about mental health outcomes among health care workers in Wuhan. In June, the published results of a survey of HCPs in New York demonstrated that psychological symptoms were common, with 57% of respondents reporting acute stress, 48% endorsing depressive symptoms, and 33% acknowledging anxiety symptoms. Lack of control, fear of transmitting COVID-19 to family, and fear for the health of family and friends were the most upsetting stressors, each endorsed by over 70% of respondents. The survey found that, while physical exercise was the most common coping strategy (59%), the majority of participants (51%) expressed interest in one or more proposed mental health wellness activities, especially online self-guided counseling with access to an individual therapist (33%) and individual counseling (28%). Some medical centers have responded by creating innovative pandemic wellness programs for their workforce, such as this one from Rush University in Chicago. They describe Wellness Rounds, a Wellness Consult Service, onsite confidential counseling, and a crisis response algorithm.
Most reports of HCP distress highlight the difficulties of working with critically ill and dying patients who are isolated from the support of their families, the fear of becoming ill or transmitting the virus to loved ones, concerns about access to PPE, and a sense of lack of control or uncertainty. An additional concern has been moral injury, which comprises the feelings of anxiety, helplessness or outrage that occur when HCPs feel unable to surmount inequities or deficiencies in the health care system, such as when shortages of PPE or other resources force HCPs to make decisions that are contrary to their commitment to healing, and awareness of how deeply rooted structural racism has made people of color especially vulnerable to the pandemic. This pre-pandemic video from Dr. Z, who is best known for his satirical raps about health care, is a profoundly serious six-minute lesson that defines moral injury and its roots in a broken health care system. The problems discussed in the video have been amplified during the pandemic. This interview looks at the effect of “moral stress” on individual HCPs and explores lessons from the pandemic about our health care system. This APA guidance document on moral injury in the pandemic is a must-read for physicians, administrators and other leaders. It asserts that, “Moral injury is associated with strong feelings of shame and guilt and with intense self-condemnation and a shattered core sense of self.” It highlights the circumstances in the current crisis that may lead to moral injury and introduces three tiers of interventions that health care systems may implement to reduce risk for such injury.
Although the literature on moral injury is primarily focused on situations in which HCPs must make decisions about treatment that are counter to their moral commitments to providing the best possible care to patients, it is showing up in a unique way right now in Colorado health care. The Department of Regulatory Agencies (DORA), the state entity that oversees all the licensing boards including the medical board, has awarded the peer health contract to Peer Assistance Services (PAS) instead of the Colorado Physician Health Program (CPHP). For background about CPHP and the importance of a confidential peer health program for physicians, physician assistants and medical trainees, please read my summer 2019 newsletter article, “Safe Haven Is Integral to Physician Wellness.” At the time of this writing, CPHP has appealed DORA’s decision and is simultaneously encouraging a public education campaign about the vital importance of confidential treatment of physicians by other physicians in order to keep the medical workforce healthy and our patients safe.
To learn more about CPHP’s campaign, check out www.PatientSafetyColorado.com, a website that outlines key issues and calls us to action. CPS’ Executive Council voted unanimously to include CPS as a supporter of confidentiality for physician treatment. On the website you will find a copy of former State Senator Irene Aguilar’s Denver Post Guest Commentary, “Doctors in crisis deserve privacy as they seek treatment” (September 2, 2020). The website also contains examples of other letters to the editor written by physicians. CPS has submitted letters to the editor as well as a longer letter to the DORA Director who oversees the Procurement and Contracts Department, the Executive Director of DORA, Governor Polis and other leaders asserting our concerns about the change in the peer assistance contract.
If you feel moved to write a letter to the editor of The Denver Post, The Boulder Daily Camera, The Colorado Springs Gazette, or your local paper, please do so. Especially if you have experience of any kind with CPHP, whether as a client, a clinician to whom they refer their clients, or a medical director who refers employees for evaluations, consider sharing your perspective about the value to the public of allowing physicians to have confidential assessment and treatment by highly vetted physicians and other clinicians. If a 150 word letter to the editor isn’t your style, please consider a Tweet: https://twitter.com/PatientSafetyCO.
In addition to this activism, there are other ways we can work to improve the mental health of our healthcare workforce during the pandemic. This thoughtful opinion piece offers strategies for maintaining resilience and optimism during this crisis. This inspiring article proposes steps forward to humanize the health care system to address the pre-pandemic problems that lead to HCP burnout. Please also check out the last two articles in the Resources for Providers list below, one on global spikes in physician burnout during the pandemic, the other on effective wellness coaching of physicians.
As psychiatrists, we are in the best position to attend to the mental health of our health care colleagues. Whether through leadership in our institutions, through our clinical activities, or through activism, we are the definitive spokespeople for the power of prevention and treatment of emotional distress. I hope each of you will join me in standing up to advocate for what we know is right, and to identify and eradicate moral injury in all its manifestations.
Stay healthy,
Claire
Claire Zilber, MD, DFAPA
CPS President
Colorado Psychiatric Society COVID-19 Resource List
September 16, 2020
Updates |
|
THANK YOU to all the CPS members (and others) who have sent in resources, written articles or reached out to us about these emails! We love hearing from you! |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
September 2, 2020
Pandemic Rage and Its Vicissitudes
Have you noticed the anger? I feel it rise in me when an unmasked stranger infringes on my personal space. I see it rise in others when I step off the sidewalk to avoid them, and they yell at me for being unfriendly. I see it everywhere in the news about protesters and counter-protesters, in political speeches, in accelerating statistics about child abuse and homicide. My topic this week is pandemic rage, which I believe flows from our collective reduced capacity to manage mounting stress, and which may be connected to increases in general hostility, domestic violence and gun violence.
There have been many descriptions of mounting anger during the pandemic. From a blog about “mom rage” to an international analysis of Twitter word clouds, which found that emotions have evolved from fear to anger as the pandemic has progressed, to an essay in Vice about pandemic-fueled hate that is just too fun a read to skip, we see many expressions of difficulty managing anger in the popular media. The scientific literature on pandemic rage so far includes a research report about increased stress and anger among youth since the pandemic began, and a Brazilian Journal of Psychiatry editorial that connects the anger to underlying fear. This interview of a Harvard psychologist also explores pandemic-related anger as a secondary manifestation of fear.
There is a lot to fear in a pandemic, and one fear that has been prominent among public health officials, mental health professionals, and advocates for women and children is a rise in domestic abuse and violence since the lockdowns began. This emergency medicine article, published in late April, describes increased reports of intimate partner violence from Wuhan, France, Cyprus and Singapore, and provides data about domestic violence reports and arrests in several US cities during the first month of lock-down. This news story describes a surge in domestic violence, including murders of women and children in the UK since March.
This trauma psychology commentary considers the surge in domestic violence during this pandemic within the context of other disasters, and suggests measures we should take, including increased funding to shelters and hotlines, heightened public and clinician recognition of domestic violence, and improved planning for women’s and children’s safety in future disasters. Those suggestions are elaborated further in this thoughtful paper about the role of psychiatry in addressing pandemic-related domestic violence. Here is an example of how a health system can directly educate the public about the intersection between domestic violence and COVID-19, including pragmatic steps a woman may take to ensure her and others’ safety. It includes a link to an app called MyPlan that offers safety plans for a variety of intimate partner violence situations, and provides assistance in assessing risks and locating resources.
It is impossible to talk about pandemic rage without also discussing firearms, which increase the lethality of all angry encounters including those in domestic violence. According to Guns Down, an American woman is fatally shot by a current or former intimate partner every 16 hours. This heart-wrenching report from the University of Pennsylvania notes that March 2020 was the worst month for gun violence in Philadelphia in the last five years, and describes the impact from the perspective of surgeons responding to gunshot wounds in the midst of a pandemic. This paper differentiates the gun buying surges this year in March and June from other such surges. An additional three million guns were sold from March through June compared to previous years. In 2020, the gun buying frenzy has been in response to the pandemic and the George Floyd (and related) protests; prior surges have been responses to uncertainty about changing gun policy.
Pandemic-fueled fear drove thousands of Coloradans to purchase guns. From March through June of this year, the Colorado Bureau of Investigations conducted over 188,000 background checks for firearm transfers, an increase of 71% over the same period last year. Ceasefire Colorado reports that between January 1st and July 31st, there have been 142 firearms homicides in Colorado, up 29% from the same period in 2019 (data from Gun Violence Archive). As of August 5th, three Colorado children died as a result of “an accidental shooting.” Two of these children were only three years old.
Widespread increases in anxiety, fear, grief, economic strain, disruptions to daily routines, and racial and economic inequities have frayed all our nerves. Friction at home, on the sidewalks, in stores, and at the workplace is higher. Physical distancing regulations, including reduced access to school, childcare and extended family members, leaves partners and parents little chance to deescalate and reset. Adding a firearm to this tinderbox increases the risk of tragedy.
What can psychiatrists do for the public, our patients and ourselves? We can continue to offer policy guidance to public officials to increase social support to families, fund mental health treatment, and enact gun reforms. We can repeat the suggestion by our pediatrician colleagues to end active shooter drills in schools during the pandemic so as not to further traumatize children. We can treat our patients with compassion for their anger, and remember to assess their risks for being the perpetrator or recipient of violence. We can check in about our own mental wellbeing, including our own degree of anger, frustration, and fear.
Those of you who know me may feel a bit incredulous that I’m ending this letter with a Christian stay-at-home-moms’ blog. The author tapped into my own truth when she wrote, “There’s something no one tells you about anger: It’s the juice. Anger has energy and power in it. You shouldn’t let it hijack you, yes. But properly directed, anger catalyzes change.” I choose the vicissitude of my pandemic rage: sublimation. Let’s use the energy of our anger, but not the venom, to fuel our responses now.
Stay healthy,
Claire Zilber, MD, DFAPA
CPS President
Colorado Psychiatric Society COVID-19 Resource List
September 2, 2020
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
August 19, 2020
Pregnancy and the Postpartum in a Pandemic
Two of my patients delivered babies in the last month, and my niece is due in a few weeks. All three women, two of them health care professionals, have had very different pregnancy and delivery experiences than they had anticipated when they first learned they were pregnant, pre-pandemic. Fortunately, all have remained physically and emotionally healthy, although two of the three have had to contend with more worry than usual. This is in contrast to the stories of three other Colorado women, each of whom had COVID-19 during their pregnancy or delivery. In this letter, I’ll summarize the known medical risks to women and babies posed by COVID-19, and then delve into the experience of pregnancy and the post-partum, including what we know so far about mental health outcomes during the pandemic.
We know that pregnancy causes changes in a woman’s immune system to reduce the likelihood of her body rejecting the fetus. This immunosuppression may increase a woman’s susceptibility to the novel coronavirus. Data from the CDC released in late June suggest that pregnant women may be more susceptible to COVID-19, and that Black and Hispanic women are disproportionately affected. Among 91,412 women of reproductive age with coronavirus infections in the first five months of 2020, the 8207 who were pregnant were 50% more likely to end up in intensive care units (ICUs) than their nonpregnant peers. Pregnant women were also 70% more likely to need ventilators, although they were no more likely to die. However, a much smaller study from Sweden cited in this article found that women with COVID-19 were nearly six times as likely to be admitted to an ICU than their nonpregnant, COVID-19-infected peers. The latter article elaborates on several possible mechanisms through which pregnant women are more susceptible to the effects of the virus.
So far, there are reassuring reports about fetal health despite the mother’s COVID-19 infection. Most babies are born uninfected and without evidence of placental infection, although there have been reports of both of those occurrences. However, because the pandemic is relatively new, we have limited data about the consequences of first trimester exposure.
Because of concern about exposing pregnant women to health care settings during the pandemic, they may have fewer in-person prenatal visits. One of my patients who had second trimester spotting struggled with the decision about whether to go in to the clinic to be checked, or stay home to protect herself and her baby from coronavirus. Reassuringly, this Mass General study found no meaningful association between the number of obstetrical visits and novel coronavirus infection.
We know that attentive prenatal care improves outcomes for women and their infants, and is one of many healthcare disparities for women from minority populations. This news story and interview discusses the pandemic’s effects on Black mothers, including their experiences of implicit bias in healthcare settings.
The pandemic has drastically changed the delivery experience as well. As outlined in this article, hospitals vary in their labor and delivery (L&D) policies depending on the status of the pandemic in their community and other factors. If a laboring woman tests positive or has symptoms suggestive of COVID, she may be allowed only one companion. Women who are not infected may be allowed more companions, but everyone must remain masked the entire time. The Colorado Department of Public Health and the Environment (CDPHE) released helpful guidance for L&D practices and breastfeeding. Earlier in the pandemic, the American Academy of Pediatrics (AAP) advised separation of potentially infected mothers from their newborns. In late July, AAP changed their recommendations to reflect recognition of the importance of breastfeeding and bonding, and the additional knowledge gained over time about the relative safety of newborns even when their mothers have COVID-19.
This article proposes areas for future research, and emphasizes the need for “mega-studies” to gather meaningful data about true incidence of maternal coronavirus infection, mother-to-child transmission, breastfeeding recommendations, long-term effects on fetal and child development, and long-term health service delivery changes. One way to gather large cohorts is through international registries, and there is now an International Registry of Coronavirus Exposure in Pregnancy.
From a medical standpoint, we now know that pregnant women are at greater risk from the coronavirus, but that their newborns are relatively safe. From a mental health perspective, the experience of pregnancy during the pandemic is complex and the issues are not yet well defined. A Canadian study found doubled rates of depression and anxiety in pregnant women in April 2020. Here is a link to the abstract, from which you may download a PDF of the entire study. Alternatively, you may prefer the news story associated with the study, which summarizes the results and suggests that social distancing may be the cause of this phenomenon, although I would add that heightened anxieties about health and the delivery could also play a role.
Becoming a new mother during a pandemic also entails disappointing changes from one’s expectations of this usually joyous time of life. This article dubs this phenomenon “social pressure shift” and offers an empathetic view of how a mother’s experience may differ from her expectations, from not having a regular baby shower, to not having parents from out of town present for the delivery, to steeply curtailed social visits after the birth. Furthermore, lactation consultants, essential resources for new moms or mothers of babies with problems latching on, are no longer as accessible. This article makes connections between the support of a lactation consultant, successful breastfeeding, infant health, and post-partum depression. I would add that frustration or failure in breastfeeding may also impact mother-infant bonding, with potential long-lasting relational impacts.
Increased stress and decreased social support may explain the rise in observed post-partum depression and anxiety since the pandemic began. Although there is no firm data yet, this news story quotes an external relations officer for a maternal mental health clinic in New York who says call volume has increased three-fold. This article by a researcher offers a sneak peek at results from a global survey of pregnant women in the pandemic. In the survey, over 70% of women reported clinically significant depression or anxiety, and over 40% screened positive for post-traumatic stress disorder (PTSD).
Psychiatrists know that maternal mental health has profound implications for child development and the mental health of subsequent generations. It is imperative that we meet maternal mental health needs during this pandemic. This article offers pragmatic suggestions for obstetricians and mental health providers, including ensuring that our patients are not being excessively strict in their physical distancing precautions to the point of isolating at home, and being proactive in our surveillance for and treatment of antenatal and postpartum psychiatric disorders. We may also guide our pregnant patients toward new resources, such as this site designed to help women identify doulas, lactation consultants and other supports in their area.
In conclusion, we are still learning about the medical and mental health implications of the COVID pandemic, but what we know so far suggests that obstetricians, pediatricians and psychiatrists must team up to bolster the safety and wellbeing of pregnant women, new mothers, and babies. We need more research, but we must not wait for the research to take action now. I am meeting more often with my pregnant and post-partum patients, emphasizing self-care and social support, helping them manage excessive anxiety, and judiciously adjusting medication when needed.
This is both a challenging and gratifying time to be a psychiatrist. Keep up your own well-being so you remain available for our important work.
My sincere gratitude goes to Kartiki Churi, MD, for assistance gathering resources for this letter.
Stay healthy,
Claire Zilber, MD, DFAPA
CPS President
Colorado Psychiatric Society COVID-19 Resource List
August 19, 2020
Updates |
|
CPS -REGISTER for PsychSummit: Psychiatry in an Evolving World - THIS SUNDAY, August 23rd from 4:30pm – 7:15pm (MST) 2.25 AMA PRA Category 1 Credits - APA Members: $20; Residents and Med Students: Free thanks to APA, Inc - Psychiatrists from across the country will come together for a three-session event on “Psychiatry in 2020”. We will begin with an exploration of technology and psychiatry through a discussion on the use of apps and other emerging tools. Turning to psychiatry’s intersection with current events, Border Mental Health will focus on the mental health challenges faced by migrants in detention and the impacts of family separation on children. Our final session will address the biggest events of 2020 head on with a live panel conversation tackling the challenges of COVID-19 and structural racism. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
August 5, 2020
The Pandemic Time Warp
Claire Zilber, MD, DFAPA
CPS President
“That really drives you insane,
Let’s do the Time Warp again.”
(The Time Warp, from Rocky Horror Picture Show)
During the first weeks of the novel coronavirus pandemic, every day seemed interminable. What I had accomplished in the morning, by evening felt like it had occurred days ago. A whole week seemed grindingly long, and the weekends fleetingly short. More accustomed now to the flow of the days and weeks, there remains a distortion about the duration of our altered lifestyle. Working from home, avoiding the gym, going grocery shopping once every two weeks, and drastically curtailing my social life seems to have been the norm almost forever, yet it’s only been five months. What’s going on?
A disconnect between objective time, measured by clocks and calendars, and subjective time, measured by our internal perceptions, has been amplified by the pandemic. Changed routines and uncertainty about the future contribute to our distorted experience of the passage of time. This article describes this phenomenon in more detail (note - the author uses the f-word once) and suggests some common-sense ways to help combat the distortion: set up a regular schedule (social rhythm therapy), change the focus of your thoughts when you find yourself ruminating (cognitive therapy), and introduce some fun (behavior therapy).
In addition to the loss of normal time flow benchmarks, the trauma of the pandemic further contributes to distorted perception of time. This article describes the psychological literature on time perception and trauma. Essentially, trauma interrupts the normal flow of time, forcing us to be hyper-focused on the present moment. “Interrupting the flow of time creates perceptual distortions such as feeling like time has stopped or that everything is in slow motion, experiencing a sense of timelessness, confusing the order of time and days, and perceiving a foreshortened future.” The authors propose specific areas of research related to the effects of distorted time perceptions in the pandemic.
Pre-pandemic research about passage of time judgements has demonstrated that positive affect and high arousal are associated with time passing more quickly than normal, whereas negative affect and low arousal are associated with time passing more slowly than normal. “Time flies when you’re having fun” is subjectively true. A British study of time perception before and after lockdown found that more than eighty percent of participants experienced changes in how quickly they perceived time passing during lockdown compared to pre-lockdown. Subjects who were older or less satisfied with their current levels of social interaction were more likely to experience slower passage of time over the course of a day or week. Higher stress and a lower task load were also associated with slower passage of time over the course of a day. The paper includes an excellent review of the psychology of time experience. If you don’t want to read the whole paper, here is its press release, which succinctly summarizes the findings.
We need additional research about the pandemic time warp. Simon Grondin, a professor of psychology at Université Laval in Québec City, and author of The Perception of Time, is conducting a study of how physical distancing may distort time perception. If you are interested in participating in the study, follow the link within this announcement.
What we know so far from psychological research is that disruption of routines, uncertainty about the future, trauma, stress, task load, age, and perhaps physical distancing all contribute to our pandemic time warp experiences. Although less scientific, this article introduces an important additional perspective to the discussion about our collective experience of distorted time during the pandemic. Optimistically, I propose that this and other lighthearted ways of viewing the pandemic will reduce stress, ease trauma, increase a feeling of social affiliation, and thereby restore more accurate perception of the passage of time.
Colorado Psychiatric Society COVID-19 Resource List
August 5, 2020
|
|
HHS - COVID-19 Public Health Emergency Extended - Declaration of Public Health Emergency for COVID-19 was extended for an additional 90 days. This renewal keeps important regulatory changes and waivers relevant to psychiatrists in effect for 90 more days (7-23-20) |
|
CPS - REGISTER for PsychSummit: Psychiatry in an Evolving World - August 23rd from 4:30pm – 7:15pm (MST) The APA has designated this live activity for a maximum of 2.25 AMA PRA Category 1 Credits (TM) - APA Members: $20; Residents and Med Students: Free thanks to APA Inc - Psychiatrists from across the country will come together for a three-session event on “Psychiatry in 2020”. We will begin with an exploration of technology and psychiatry through a discussion on the use of apps and other emerging tools. Turning to psychiatry’s intersection with current events, Border Mental Health will focus on the mental health challenges faced by migrants in detention and the impacts of family separation on children. Our final session will address the biggest events of 2020 head on with a live panel conversation tackling the challenges of COVID-19 and structural racism. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
July 22, 2020
To School or Not to School?
Dear Colleagues,
So many opinions, so few data points. The news is full of conflicting recommendations from the Administration, health care organizations, teachers, parents and pundits. In this letter you will find scientific data about SARS-CoV-2 transmission in pediatric populations, as well as clarification of the position statements of various healthcare organizations. This may assist you in conversations with your patients or their parents to help them determine the most appropriate solution as they consider their options.
One concern about allowing children back to school is that they will bring the virus home to more vulnerable members of the household. As explored in this Kaiser Family Foundation report, 6% of US seniors live in homes with school-aged children. Initial data from China and this more recent report from Switzerland suggest that most children have mild or asymptomatic illness, and that transmission within family clusters is much more likely to be from adult to child than the other way around. In only 8% of households did children develop symptoms before others in the home. That reassuring news is offset by a Korean study that suggests that older children (ages 10-19) may spread the virus to household members more readily than adults do. They followed nearly 60,000 contacts of 5700 COVID-19 index patients for roughly 10 days. Their findings included that 12% of household contacts were infected, versus 2% of non-household contacts. When the index patient was aged 10–19 years, 19% of household contacts were infected. In contrast, when the index patient was aged 30–49, 12% of household members were infected, and when the index patient was aged 0–9 years, just 5% of household contacts were infected. The authors acknowledge that they "could not determine direction of transmission."
A second concern is that a small number of children who are infected with the virus develop an inflammatory multisystem syndrome with presentations ranging from fever and inflammation to myocardial injury, shock, and development of coronary artery aneurysms. Of course, no parent wants to risk such a serious outcome for their child, but we must remember that this is an exceedingly rare occurrence. This JAMA editorial, Should Coronavirus Disease 2019–Associated Inflammatory Syndromes in Children Affect Social Reintegration?, argues that we should not allow fear of a condition that may affect hundreds be a basis for restricting millions of children from school. This public health approach is rational but may be difficult to apply when dealing with parents’ emotional, protective instincts.
More convincing may be data about the pandemic effects on kids’ social and emotional health. This report from China, Behavioral and Emotional Disorders in Children During the COVID-19 Pandemic, describes a preliminary study of children’s responses during the lockdown phase of the pandemic response. They found high rates of clinginess, fear of infection, inattention, irritability, sleep disorders, nightmares and other symptoms indicative of stress. As psychiatrists, we are already aware of the importance of daily routines, social bonds with classmates, and mentorship from teachers and coaches. These experiences, all provided by school, help children develop self-regulation and self-esteem. We know that when these processes are interrupted by abuse, neglect or serious medical illness, the child’s developmental trajectory is thrown off course. What we don’t know is what happens when an entire population of children experience massive stressful disruption all at the same time. From this perspective, a return to school feels like it could be protective, but that is conjecture, not data.
Another argument for returning to school is concern about the impact of remote learning on academic “health,” especially for students with home environments that aren’t able to provide access to technology or to the calm and structure that promotes learning. This NYT article describes several studies of academic progress during springtime lockdowns that showed loss of academic skills, particularly among students from less privileged zip codes. Can our society afford to allow disparities in education to get larger than they already are, especially now that we are more acutely aware of the history and consequences of these disparities?
The question about whether and under what conditions schools should reopen has become a political hot button recently as the White House and the CDC have publicly disagreed, as seen for example in this CNN report. The CDC, whose mission is to prevent the spread of disease, takes the position that remote learning is safest, but they also offer pages of guidance to parents, teachers and school administrators about how to be safer while in school.
In contrast, The American Academy of Pediatrics (AAP) has recommended that schools reopen in August so that students can be “physically present in school” as much as possible. AAP’s recommendation to reopen schools is based on concern that continuing remote learning is likely to result in severe learning loss, an increase in mental health symptoms, an increase in both physical and sexual child abuse, an increase in adolescent substance use, and an increase in suicide. AAP reports that they have already seen some of these outcomes in children and adolescents between March and May 2020 when school was remote.
This interview with Dr. Sean O’Leary, a pediatrician at CU Anschutz, a father of two teens, a survivor of COVID-19, and one of the authors of the AAP position statement, illuminates the balance pediatricians are trying to strike between emerging knowledge about the impact of distance learning and the risk of COVID-19 transmission by children.
As a result of this recommendation by the AAP, Denver Public Schools was considering reopening in August, with precautions. However, after meeting with health officials from Denver Health, they announced that they will delay in-person learning. The first day of school will be August 24, but it will be in a remote learning format. They will consider a gradual return to in-person learning starting September 8.
The APA and AACAP (American Academy of Child and Adolescent Psychiatry) issued a joint statement supporting the reopening of schools if possible, and highlighting the importance of social interactions for healthy development, the need for adaptive techniques for some students to learn remotely, and the role of mental wellbeing for students, teachers and parents.
The two largest organizations representing teachers, the American Federation of Teachers (AFT is the teachers’ union) and the Association of American Educators (AAE is non-union), have websites rich with COVID-19 related resources. The AFT website includes a plan for reopening schools. The AAE website has an interesting report on results of their springtime teacher survey about COVID-19. One striking finding is that 84% of responding teachers agreed with school closure.
Teachers do more than educate. One of their roles is to monitor the health of children in the classroom, including for signs of child abuse and neglect. Ordinarily, 20% of abuse and neglect reports come from teachers. This paper highlights concerns about increased child abuse and neglect during the pandemic, combined with less reporting of such abuse because children are not in school.
Schools do more than educate. They provide a safe space, a daily meal (sometimes two, if breakfast is provided), opportunities to form friendships with peers, interaction with caring adults, and access to school nurses and mental health counselors. This thoughtful interview with psychologist Elena Hontoria Tuerk about supporting children’s development during the pandemic addresses many of these important functions of schools, as well as the importance to parents of having a break from their children.
One group of students about which I am especially concerned are LGBTQ youth. Many of these kids aren’t safe coming out to their parents and they rely on peers for crucial support. These children are at higher risk than others for physical abuse, homelessness and suicide. What will they do without the community support and counseling found at school?
There are so many other special populations of students. Children with asthma, cancer, cardiac defects, cystic fibrosis or other chronic medical conditions that place them at higher risk need education, too, but the health risks for them to return to the classroom are higher. As we saw this spring, parents who are trying to work from home and simultaneously teach their children are inordinately stressed. What do these parents do if they are required to return to the workplace? Children with special developmental needs may be in an even more precarious position without the structure, specialized instruction and support of school.
There are no simple answers. Alex de Tocqueville wrote, “The public will believe a simple lie rather than a complex truth.” It is facile to make sweeping statements that “all schools should reopen,” or “all children should return to the physical classroom.” Each child exists within a unique family, which lives in its unique community, which has its unique experience with the pandemic. When and how to return to the classroom ought to be an individualized decision based on each child’s needs. Unfortunately, insufficient resources may force school districts into a one-size-fits-all strategy. Psychiatrists cannot singlehandedly resolve the policy differences of the various entities involved in this debate. What we can do is help our patients find the best solutions for themselves, guiding them towards rational rather than emotional decision-making.
Stay healthy,
Claire Zilber, MD, DFAPA
CPS President
Colorado Psychiatric Society COVID-19 Resource List
July 22, 2020
Updates |
|
Notice - There will not be a CPS COVID-19 Resource Email sent next Wednesday, July 29th. You can expect an email in your inbox again on Wednesday, August 5th. |
|
CPS - REGISTER for PsychSummit: Psychiatry in an Evolving World - August 23rd from 4:30pm – 7:15pm (MST) - Psychiatrists from across the country will come together for a three-session event on psychiatry in 2020. We will begin with an exploration of technology and psychiatry through a discussion on the use of apps and other emerging tools like digital tracking for medication adherence. Turning to psychiatry’s intersection with current events, Border Mental Health will focus on the mental health challenges faced by migrants in detention and the impacts of family separation on children. Our final session will address the biggest events of 2020 head on with a live panel conversation tackling the challenges of COVID-19 and structural racism. |
|
CO Mask Mandate - Executive Order D 2020 138 is a mandatory statewide mask order that went into effect at midnight on July 16, 2020, and will be in effect for 30 days. It may be extended. Also see CPR - Colorado Mask Order: When Do I Need To Wear A Face Covering? (And More Mask Questions Answered) and CDPHE - Questions & answers about the mask order. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
July 15, 2020 *Special Edition*
Psychiatrist Resources on Historically Marginalized Communities
To see past resource lists for psychiatrist and messages from CPS Presidents, visit https://www.coloradopsychiatric.org/COVID19
To explore the COVID-19 Resource Page for the Public, visit https://www.coloradopsychiatric.org/coronavirus
Do you have a question, helpful resource, or tip for your colleagues? Email [email protected].
Welcome to this special edition of the CPS COVID-19 Resource Email!
CPS has received resources from members concerning racism and the pandemic as well as more general resources on racism and psychiatry so we have decided to dedicate this edition of the CPS COVID-19 Resource Email to the topic. The first section contains resources and articles on the intersection between COVID-19 and historically marginalized communities. The second section focuses on resources for psychiatrists to help us better serve patients with skill and sensitivity, as well as resources for psychiatrists from historically marginalized communities.
|
PsychSummit: Psychiatry in an Evolving World - registration opening soon Psychiatrists from across the country begin the three-session event with an exploration of technology and psychiatry through a discussion on the use of apps and other emerging tools like digital tracking for medication adherence. Turning to psychiatry’s intersection with current events, Border Mental Health will focus on the mental health challenges faced by migrants in detention and the impacts of family separation on children. Our final session will cover COVID-19 and structural racism. |
Colorado Psychiatric Society COVID-19 Resource List
*SPECIAL EDITION*
July 15, 2020
|
|
For the most complete and up-to-date race and ethnicity data on COVID-19 in the United States, see The COVID Racial Data Tracker - a collaboration between the COVID Tracking Project and the Boston University Center for Antiracist Research. Also see NYT - The Fullest Look Yet at the Racial Inequity of Coronavirus - New data — made available after The New York Times sued the federal government — shows the extent of racial disparities: The contraction rate is almost three times as high for Black Americans as white Americans and more than three times higher among Latinos than whites. |
|
CDC webpage on COVID-19 in Racial and Ethnic Minority Groups - contains data, recommendations on what healthcare systems and healthcare providers can do and discussion of factors that explain why racial and ethnic minority groups are at increased risk during COVID-19 (6-25-20) |
|
JAMA - Taking a Closer Look at COVID-19, Healthcare Inequities and Racism (transcript article and 31 minute video) (6-29-20) |
|
NIH - Director Francis Collins, MD, PhD, discusses the heartbreaking disproportionate impact of COVID-19 on Black and Hispanic communities and the importance of building stronger relationships with minority communities to build trust as COVID-19 vaccine development progresses (see article not 2 minute video) (6-23-20). Also see STAT - COVID-19 Vaccine Research Must Involve Black and Latinx Participants. Here are 4 Ways to Make That Happen (6-26-20) |
|
Virtual Forum: Healthcare Disparities through the Lens of Diversity During the COVID-19 Pandemic (slidedeck (download) and 2 hour 17 minute video) - AACAP hosted this virtual forum on June 13 highlighting mental health, COVID, and other healthcare disparities related to race and ethnicity among children and adolescents of color. |
|
New York Times - The Challenges of the Pandemic for Queer Youth - Issues include limited access to community support and counseling and, in some cases, quarantining with unsupportive family members (6-29-20) |
|
PsychNews - Hispanic Community and COVID-19: Addressing Health Inequalities Can No Longer Be Delayed (6-23-20). Also see NYT - Many Latinos Couldn’t Stay Home. Now Virus Cases Are Soaring in the Community (6-26-20) |
|
AMA - Widening Social and Health Inequalities During the COVID-19 Pandemic (6-10-20) |
|
JAMA - Strategies for Digital Care of Vulnerable Patients in a COVID-19 World—Keeping in Touch - Without action to address the digital divide, existing health and healthcare disparities will be exacerbated for the nation’s most vulnerable individuals and communities. Article explores these potential dangers and offers strategies to mitigate them (6-12-20) |
| KFF - Chart of the Week: The Disproportionate Impact of COVID-19 on Black and Hispanic Medicare Recipients (6-26-20) |
| Hopkins Bloomberg Public Health Magazine - Racism and COVID-19 - In this Q&A, Lisa Cooper, a practicing physician and epidemiologist, discusses racism’s role in COVID-19 cases in African American communities and solutions for the inequities. |
| AMA Ethics - Ethics Talk: Antiracism, Health Equity, and a Post-COVID Future (22 minute podcast) - AMA Ethics Journal editor in chief, Dr Audiey Kao, talks with Dr Ibram Kendi, founding director of the Antiracist Research and Policy Center and a professor of history and international relations at American University, about the impact of racist policies on historically discriminated-against groups and what it means to be an antiracist (06-20). Kendi uses the metaphor of cancer and its treatment to discuss racism and anti-racism. He also addresses the importance of antiracism among healthcare providers in order to appropriately address health disparities. Of special interest is a section towards the end (approx. minutes 17-19) about the difference between truth and lies, and why it’s so difficult to communicate complicated truths to people who prefer simple one-liner answers. |
| JAMA - COVID-19 Pandemic, Unemployment, and Civil Unrest: Underlying Deep Racial and Socioeconomic Divides (6-12-20) |
|
|
Selected APA Resources:
|
|
American Association For Community Psychiatry - The Leadership Role of Community Psychiatry in Combating Structural Racism (1 hour video) (6-3-20). Many excellent speakers, including a presentation by Dr. Shim on structural racism (starting around minute 6). Also see her article in Stat - Structural racism is why I’m leaving organized psychiatry - a piece by Ruth S. Shim on why she has made the difficult decision to end her membership with organized psychiatry, specifically the American Psychiatric Association (7-1-20) |
|
Taking Back Our Voices — #HumanityIsOurLane by psychiatry resident Chase T.M. Anderson, M.D. (6-30-20) - Also see Race and Medicine on NEJM.org - a new page presents a selection of articles on race and medicine, with implications for improving patient care, professional training, research, and public health. |
|
Treating Mental Health in the Black Community (1.5 hour video) - Learn how you can better serve Black clients (6-9-20) |
|
Kevin MD - A physician awakens to racism in America (6-15-20) |
|
MD Edge/Clinical Psychiatry News - Examining bias (6-18-20), includes link to Harvard researcher designed Implicit Association Test. |
|
75 Things White People Can Do for Racial Justice (the list now includes 97 things!) |
|
On Being with Krista Tippett - ‘Notice the Rage; Notice the Silence’ (51 minute podcast) - The best laws and diversity training have not gotten us anywhere near where we want to go. Therapist and trauma specialist Resmaa Menakem is working with old wisdom and very new science about our bodies and nervous systems, and all we condense into the word “race” (6-4-20). Visit https://www.educationforracialequity.com/resmaa for details on a two session online event on July 25th and August 1 - Reclaiming our Birthright: An Embodied Gathering for Black Men held by Resmaa Menakem and Dr. Kenneth Hardy as well as other events. Also see https://www.resmaa.com/. |
|
Focus - Trauma-Informed Care and Cultural Humility in the Mental Health Care of People From Minoritized Communities (download - open with PDF reader) Dr. Ranjbar is a panelist at the upcoming CPS PsychSummit event! |
| Focus - Diversity and Inclusion in Psychiatry: The Pursuit of Health Equity (download - open with PDF reader) (6-24-20) |
|
Focus - Affirmative Care Across Cultures: Broadening Application (download - open with PDF reader) - recommendations for affirmative care in practice with African-American, Asian, Indigenous, and Latinx individuals, as well as those living in rural communities.) |
| MD Edge/Clinical Psychiatry News - How can we better engage black men as patients? (6-24-20) |
| MD Edge/Clinical Psychiatry News - Management of race in psychotherapy and supervision (6-22-20) Dr. Isom is a panelist at the upcoming CPS PsychSummit event! |
| HHS - National CLAS Standards - The National Culturally and Linguistically Appropriate Services Standards are a set of 15 action steps intended to advance health equity, improve quality, and help eliminate health care disparities by providing a blueprint for individuals and health and health care organizations to implement culturally and linguistically appropriate services. If the website is not loading, click here. Also see HHS - Improving Cultural Competency for Behavioral Health Professionals (Free Online Training - This program is accredited for 4 – 5.5 contact hours for psychiatrists) |
| Dismantle Collective - White Allyship 101 (list of articles and books). Also see Power Shift Collective - Checklist for White Allies |
| Psychology Today - Uncovering the Trauma of Racism - includes new tools for clinicians and examples of race-related traumas that may meet DSM-5 criteria for PTSD. |
| MD Edge - The fallout from George Floyd's death: Physicians, how are you? How are your patients? A conversation on race for psychiatrists (45 minute podcast) - Lorenzo Norris, MD, welcomes fourth-year psychiatry resident Brandon C. Newsome, MD, for a discussion on race relations as a physician in the wake of the death of George Floyd. The pair discuss what their patients are experiencing and what they're experiencing as black physicians (6-5-20). Transcript available at George Floyd, race, and psychiatry: How to talk to patients (6-24-20) |
| NPR - 'Bear Our Pain': The Plea For More Black Mental Health Workers (article and 4 minute audio) (6-25-20, aired 6-6-20) |
| HuffPost - This Is What Racial Trauma Does To The Body And Brain Racism, injustice and brutality — experienced directly and indirectly — can have a lasting effect on a person's mental health (7-1-20) |
| MBK Alliance Town Hall Series: Mental Health and Wellness in a Racism Pandemic (1 hour video) - President Obama joined Congressman John Lewis, founder and executive director of the Equal Justice Initiative Bryan Stevenson, writer and survivor of police brutality Leon Ford, Jr., and youth leader LeQuan Muhammad, in a conversation moderated by activist and author Darnell Moore, to discuss the mental toll racism takes on people of color. |
| HuffPost - One Way To Be An Ally Right Now? Support Black Mental Health (updated 6-18-20) |
| HuffPost - Racism Is A Mental Health Crisis. Here's How To Fight It. - “Being a Black person is often described as being in “fight or flight” mode, and honestly, that is the best way to explain it.” (6-11-20) |
| HuffPost - What Not To Say To Someone Who Has Experienced Racial Trauma (article and 5 minute video) - What white people and other allies do in conversations about the mental health effects of racism matters (7-3-20) |
| YoungMinds - How racism impacts my mental health - Sian, 19, shares how racism affects her mental health, and what helps her cope - watch movies with more Black people, or follow Black YouTubers or influencers. This will just make you feel more comfortable with seeing Black people and, eventually and maybe subconsciously, you will learn to love yourself and what you are.(6-23-20) Also explore the Good Black News website. |
| Psychology Today - Is Your Therapist Qualified to Treat People of Color? Ten questions that all culturally-informed therapists should be able to answer (5-31-19) |
| Ourselves Black - Racial Inequality, Police Brutality & Black Mental Health (56 minute video) - presentations by two young black male psychiatrists - Dr. Christopher Hoffman and Dr. Walter E. Wilson, Jr. |
| Kevin MD - How racial issues affect both doctors and patients (11 minute podcast) (6-25-20) |
| KFF - Officials Seek To Shift Resources Away From Policing To Address Black ‘Public Health Crisis’ - on declaring racism a public health crisis (6-25-20) |
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
PsychSummit: COVID-19
PsychSummit: COVID-19 includes an interview with APA President Bruce J. Schwartz, MD, on his experience on the ground in the epicenter and takeaways for psychiatrists in other states and see glimpses into the lives of NYC New York psychiatrists during COVID-19. PsychSummit is a partnership between the Colorado Psychiatric Society and the New York County Psychiatric Society. From the beginning it has been a VIRTUAL INTERACTIVE conference designed to bring together psychiatrists from across the country (and beyond) to discuss some of the most pressing issues the profession faces. www.PsychSummit.org
July 8, 2020
Neuropsychiatric Sequelae of COVID-19
Dear Colleagues,
The planet is eight months into the pandemic, and although it’s been only four months in Colorado, the only other four months that felt this long to me were those in the second half of my pregnancy. It is not news to any of us that there are psychiatric sequelae of living in a pandemic. We are all aware of surges in depression, anxiety, trauma-related symptoms and substance use. What is less clear are the neuropsychiatric sequelae of COVID-19. Information emerging from Wuhan and other early centers of the pandemic, as well as research on prior coronavirus pandemics, begins to suggest a picture of both direct, virally-mediated neuropsychiatric illness, and illness mediated by immunological or other host responses to infection. Although we are at the stage where there are more questions than answers, this letter will provide a summary of the current state of knowledge.
There are several case series of patients with COVID-19 that describe neurological symptoms. This series of 214 patients in Wuhan, China, describes cerebrovascular events and impaired consciousness in 45.5% of patients with severe infection. A review of 27 autopsies of patients who died from COVID-19 in Germany describes detecting the virus in multiple organs, including the brain. This brief report details neurologic findings in a case series of four pediatric cases with multi-system inflammatory syndrome from COVID-19. The most common neurologic complaints in COVID-19 are anosmia, ageusia, and headache, but stroke, impairment of consciousness, seizure, and encephalopathy have also been reported. It may be that the encephalopathy results from toxic-metabolic factors (cytokine storm, inflammation, renal dysfunction, etc.) rather than directly from the virus. This review article on neuropathogenesis and neurologic manifestations of COVID-19 goes into more depth.
While many have reported that COVID-19 patients have experienced vascular and neurological problems, a recent study of 153 patients in Lancet Psychiatry reports that patients are also showing symptoms of psychiatric disorders, including psychosis and depression. The British researchers found that 77 patients experienced a cerebrovascular event (primarily stroke), 39 experienced altered mental status, six experienced peripheral nervous system problems, and three experienced other nervous system–related complications. Among the 39 patients with altered mental status, 16 were diagnosed with encephalopathy, and 23 were diagnosed with a psychiatric disorder. Ten of these 23 patients developed psychosis, six developed cognitive problems, and seven developed mood problems including depression and mania. One striking finding is that the neuropsychiatric manifestation may differ according to the patient’s age. Specifically, 49% of the patients who experienced altered mental status were under age 60, whereas 82% of patients who experienced a cerebrovascular event were over age 60.
Past coronavirus epidemics, including SARS (2002) and MERS (2012), may shed light on the current pandemic. Based on their review of the literature on psychiatric and neuropsychiatric presentations during prior coronavirus outbreaks, these authors opine that SARS-CoV-2 may cause delirium in a significant proportion of acutely ill patients. They also warn about the possibility of depression, anxiety, fatigue, post-traumatic stress disorder, and rarer neuropsychiatric syndromes in the longer term.
This excellent review discusses the psychological, neurological, and neuropsychiatric manifestations that COVID-19 may take, as well as addressing some of the potential immunologic mechanisms for the symptoms. Importantly, the authors remind us of the association between maternal influenza and subsequent development of schizophrenia in offspring. They warn us that we may see a late wave of neurological (eg: Parkinson’s disease) or psychotic illness decades after the pandemic.
Most of the neuropsychiatric illness seen in patients with COVID-19 is probably due to delirium or other encephalopathic states caused by the inflammatory response, metabolic toxicities or hypoxia. However, it is possible that some neuropsychiatric manifestations could be caused directly by the virus. SARS-CoV-2 uses spike proteins on the viral surface to bind to angiotensin converting enzyme 2 (ACE2) receptors on host cells. Humans have ACE2 receptors on airway epithelia, kidney cells, small intestine, lung parenchyma, and vascular endothelia throughout the body. ACE2 receptors are also found on neurons, astrocytes, and oligodendrocytes, and are highly concentrated in the substantia nigra, ventricles, middle temporal gyrus, posterior cingulate cortex, and olfactory bulb. As detailed in this article, it remains unclear whether the virus directly attacks neural tissues; although isolated case reports suggest it may, others suggest the neurologic effects are a result of cytokines (headaches), hypercoagulability (strokes) or other secondary factors.
If you only have time to click on one link in this letter, choose this outstanding and comprehensive article, which includes helpful, colorful diagrams explaining possible mechanisms of pathogenesis. You may feel like you’re back in medical school. Helpfully, toward the end of the article the author describes the roles psychiatrists may play in the pandemic, and suggests pragmatic treatment considerations such as drug-drug interactions between psychotropic medications and antivirals.
We have learned a lot, but there is so much more to learn. This brief report calls for long term study of the neuropsychiatric outcomes of the pandemic. Ultimately, we need prospective studies of neuropsychiatric illness in COVID-19, including long-term outcomes, to fully understand the nature of this beast.
Stay healthy,
Claire Zilber, MD, DFAPA
CPS President
Colorado Psychiatric Society COVID-19 Resource List
July 8, 2020
|
|
APA Survey to inform the work of the new Presidential Task Force to Address Structural Racism Throughout Psychiatry. Please complete the short survey by Friday, July 10th. Please note that the survey is a Google Form, so if individuals cannot access it through their institution’s servers, it can be completed at home. Answers will be anonymous and not shared on this platform. |
|
Partnership COVID-19 Document (download) - CPS is a founding member of the Behavioral Health Partnership, a long-standing group of stakeholders made up of consumer and provider organizations in Colorado. The group has created a COVID-19 document for the public on steps we can all take to ensure we are caring for our mental wellbeing. Please share with patients, family, friends and anyone else who may find it helpful. |
|
|
|
|
|
JAMA - Attitudes and Psychological Factors Associated With News Monitoring, Social Distancing, Disinfecting, and Hoarding Behaviors Among US Adolescents During the Coronavirus Disease 2019 Pandemic (6-29-20) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
July 1, 2020
Zoom Fatigue
Dear Colleagues,
We would be having a very different pandemic experience if not for videoconference technology. Three hundred million people attended meetings through Zoom in April of this year, compared with ten million people at the end of 2019. Psychiatrists have adopted telepsychiatry en masse as a result of the pandemic, and we have enjoyed the smallest reduction in visits of all ambulatory medical practices. We also may reap some benefits from doing telehealth from home: more time with family members and pets, less time in traffic, healthier lunches, and the ability to start a load of laundry between appointments. Despite these and other efficiencies, many of us feel more drained at the end of the day. In this letter I explore the reasons for “Zoom fatigue” and share some potential strategies to help manage it.
Social science research informs us that interactions by videocall are not the same as those in person. Our brains evolved to see the entire human form in three-dimensional space, not a two-dimensional disembodied head and shoulders. Research shows that video calls disrupt the pattern of communication we have developed over millennia for our survival. Normal human communication requires a complex synchrony between each person’s spoken words, gestures, and body movements. Synchrony may be somewhat achievable over video, but the lag in transmission between visual and audio, as well as reduced nonverbal cues make it more difficult. We are left over-focusing on words, which can be especially exhausting if the audio connection is fuzzy. Multi-person video meetings magnify this phenomenon, challenging the brain’s central vision by trying to focus on a gallery of participants. It’s a new kind of multitasking for which our brains are not designed. In addition, the constant eye contact invited by a video call requires extra energy and can feel unnerving. I have had at least one patient exclaim, “Stop staring at me!”
In addition to neurologically derived difficulties with video calls there are psychological and social reasons that we may feel exhausted after a day of interacting this way. As we try to look into our patient’s eyes, we know we are not actually looking in their eyes. We are looking at an image of their face on the screen or looking at the camera. This sets up a kind of cognitive dissonance: I’m connecting yet not really connected. Interacting only on a screen means we lose the energy boost that we might ordinarily get when we break up the day by meeting someone for coffee or greeting a colleague in the hallway. Also, it’s not normal behavior to smile all the time, but in a video meeting, especially with the thumbnail image of ourselves in the upper right corner, we may feel self-conscious about needing to smile.
Psychiatrists are fortunate that we can rely on video calls for much of our work; however, telehealth may exacerbate problems inherent to the practice of psychiatry. Ours is largely a solitary profession. Whether employed by an academic medical center, a community mental health clinic or in private practice, we spend much of our time seeing patients alone in our offices. Telehealth may further isolate us from our colleagues. We may have difficulty creating reasonable separation between work and home tasks if we are working from our dining room or home office. This article was written before the pandemic, yet it speaks in relevant ways to both the potential benefits and pitfalls of telehealth for psychiatrists.
How might we modify our telehealth protocols to mitigate the exhaustion? This PsychNews article has seven simple and pragmatic suggestions for our professional videocalls. We might also try to differentiate professional videocalls from personal ones. For example, I use DoxyMe only for my clinical work, and rely on Zoom or FaceTime for personal events. I hold my professional calls in the same two locations (depending on whether I need to be plugged in to ethernet or if wifi is good enough). I avoid these two settings for personal calls. I dress up in work attire for my professional work day, just as if I were going into my office. To give myself a break, I decline some requests for social Zoom events, which is tricky to do without hurting feelings; this article offers some tips. Read the section toward the end of this article on “how to dial it back” for some creative ways to rest our brains from excessive screen time.
This, too, shall pass. One day, we will all be back in our offices or clinics or ERs or wherever we work, seeing patients face to face, touching their arms as we examine for dystonia, passing a box of tissues with which to wipe their tears. Some of us may choose to continue to use telehealth some or all of the time, but it will be a choice, not a requirement. In his 1996 novel, Infinite Jest, David Foster Wallace imagines a future in which videophones are invented. Initially met with enthusiasm, then adapting with slightly improved resin masks of their own faces so they can look better during calls (there’s a setting for that in Zoom, by the way), then fatigue, the trend collapses after a year, and everyone goes back to audio-only calls. For now, I choose to adapt with humor:
Stay healthy,
Claire Zilber, MD, DFAPA
CPS President
Colorado Psychiatric Society COVID-19 Resource List
July 1, 2020
Updates |
|
NEW Section on CPS website - CPS has added a new section on Racial and Ethnic Minority Community Issues to our COVID-19 Resource documents - see below or visit Resources for the Public. We will also be adding a new section with resources for psychiatrists. If you know of any resources that would be helpful, please send them to [email protected]. |
|
|
|
|
|
Amid pandemic, prison psychiatrists adjust and persist (6-22-20) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
June 24, 2020
Loneliness
Dear Colleagues,
Now into our fourth month of the pandemic lifestyle, the novelty has worn thin. The trips I had planned for 2020 are all cancelled, the long-weekend family reunion to celebrate a speed-limit birthday (although the only place in the country you may go this fast legally is on Texas State Highway 130) has been replaced by a 90 minute Zoom call, and annual traditions with friends are scrapped. The most difficult part for me is not knowing when I will see certain people again. I realize I am lucky: I live with a partner I love and the best dog in the universe. The pandemic is creating unprecedented disruption in social connectedness for all of us, but especially for those who live alone. I am particularly concerned about seniors and adolescents.
Earlier in the pandemic, 13.6% of U.S. adults reported symptoms of serious psychological distress, which is three times higher than two years before (3.9%), according to a recent survey. Among respondents age 18-26, 34% reported distress in April 2020, compared to only 3.7% in April 2018, a nine-fold increase. Paradoxically, loneliness tripled among those who live with others and “only” doubled among those who live alone. This highlights the importance of National Institute of Aging research demonstrating that social isolation and loneliness, although connected, are not equivalent.
A Harris Poll commissioned by 4-H in May asked 1,500 youth about their mental health. Among the results: 61% said that the pandemic has increased their feelings of loneliness, 55% reported anxiety, 43% reported depression, and 64% believed the pandemic will have a lasting impact on their generation’s mental health. The teens surveyed also reported that they spend 75% of their waking hours on screens. It will be interesting to see if screen time drops now that school is out for the summer. As psychiatrists, we all know that excessive screen time is associated with adverse outcomes for children and adolescents, particularly with regard to diet, weight, depressive symptoms and quality of life.
Solutions for adolescents may be relatively easy to negotiate, to the extent that one is able to negotiate with a given adolescent. CPS has gathered an impressive collection of activities for families and children to help engage youth in non-screen activities. Please encourage your patients to check out the links on our Resources for the Public webpage. Many parents of adolescents have decided to bend the rules for their kids, allowing them to venture out with their friends because of a recognition that social groups and friendships are like air and water for teens.
Among the resources missing from many children’s lives during the pandemic are their grandparents. There are countless heart-wrenching news stories about family members trying to connect with elders quarantined in nursing homes. Although the need for quarantine is understandable if the goal is isolation of the virus, the rigidity of the quarantine suggests that policy makers have lost sight of the larger picture of health for people living in nursing facilities. To lock an elderly person in a room with almost no human interaction is to invite cognitive, emotional and physical decline. Think about what we know about solitary confinement. Even elders who live independently are exhorted to maintain strict shelter-in-place protocols as the rest of society opens up a bit. Long before the pandemic, we knew that social isolation can induce depression, reduce immune function, increase oxidative stress and is associated with dementia in seniors.
Humans evolved as social animals. We need interpersonal connection for our very survival. Loneliness is harmful, and loneliness during a period of increased stress because of a deadly virus and social upheaval may be especially burdensome. This paper on the Neurobiology of Social Distance is the best I have found, and worth the time to read. For a shorter version, this commentary piece by Dr. Richard Friedman is a less academic discussion of the effects of social isolation on cognition.
Have we created a false binary: seniors must be completely isolated or else they risk dying from the virus? Could we imagine responsible ways to soften the degree of isolation without sacrificing safety? How might psychiatrists join the public health conversation about the way we’re treating our seniors? This call for research on combating loneliness contains excellent ideas, including for individual and societal interventions. The UK has created a “Campaign to End Loneliness;” the website includes some charming short videos about talking to strangers, making friends, and other forms of connection.
Perhaps the pandemic will be a catalyst for reprioritizing where we place our elders in the social fabric, recognizing the importance of the multigenerational family, and rethinking public policy to be more relationship-centered.
Stay healthy,
Claire Zilber, MD, DFAPA
CPS President
Colorado Psychiatric Society COVID-19 Resource List
June 24, 2020
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
June 17, 2020
Twin Pandemics
Dear Colleagues,
We are in the grip of twin pandemics: coronavirus and racism. One has been in the US for five months, the other for over 400 years. The emotional toll of the former has amplified the urgency of the response to the latter so that finally, finally our country is paying attention to what Black people have been telling us for years. Rosa Parks refused to give up her seat on a Montgomery bus 65 years ago. This iconic moment happened before most of us were born, which means visible, well-publicized struggle for equality has been going on our entire lives and we have not been paying enough attention. This letter will focus on the mental health toll of both COVID-19 and racism on the Black community, and on what we as psychiatrists must do to help.
It is well documented that Black, Native American, Latinix and other minority populations have been disproportionately affected by COVID-19. This CDC page explores factors that contribute to disparities in health during the pandemic, as well as advice to health care professionals and health care systems for addressing the problem. Because Black people are dying at a higher rate, Black families are experiencing more grief and loss. At the same time, Black families often have more difficulty adapting to the pandemic because their socioeconomic situation leaves them with fewer options. Although a common response to the pandemic is that “we’re all in this together,” the truth is that we are not all having the same experience. This British article expounds upon COVID-19 as “the great unequalizer.”
The pandemic and its resulting unemployment are inextricably connected to the current civil unrest in response to ongoing police murders of Black individuals, as articulated in this article in JAMA. Black people are feeling assaulted by simultaneous medical and existential threats, and the long term mental health effects of this level of trauma must be considered. A CDC survey cited here found that Black adults currently report more psychological distress, with 45% reporting anxiety or depression in the week following George Floyd’s killing, compared to 33% of white people. Historically, Black people have had less access to and less trust in mental health treatment, and they may experience more stigma about seeking psychiatric care. If we are to support the Black community through these twin pandemics, we must support its mental health.
What can we do and where do we start? We must work harder to make health care settings welcoming and safe environments for Black patients and providers. We must speak up when we witness race-based humiliation, exclusion, invalidation or aggression. Psychiatrists can promote healing when treating patients who have experienced trauma by adopting a trauma-informed care approach and an attitude of cultural humility.
Part of our cultural humility must include an openness to learning more about race and racist oppression. APA’s President and four distinguished speakers met June 15th in a webinar focused on structural racism and the way forward. A recording is now available for APA Members. If you did not attend the webinar, I suggest you carve out an hour and do so this week. It should be mandatory watching forany psychiatrist who wants a deeper understanding of the experience of Black psychiatrists in our training programs, hospitals, and organizations.
Four books were recommended during the webinar: White Fragility, Medical Apartheid, So You Want To Talk About Race? and Racism & Psychiatry. You may also read the statement on domestic terrorism and violence in America found on the Black Psychiatrists of America website. I also intend to spend more time on the Race & Medicine website, especially this page of resources for white physicians to use to delve deeper to understand privilege, bias, and how we can help address the racism we witness.
We must promote more equity in medical research. The exclusion of minorities from genomic testing has healthcare implications; although only 16% of the world’s population are descendants of Europeans, 78% of genomic testing used in the genome-wide association study is from people of European descent. We are basing medical research on a small segment of the human population with the arrogance of the white, European “majority” that we are all we need to know about.
As individuals and as a profession, we must take responsibility for the problem of racism in America and in healthcare. I welcome your suggestions for actions CPS and the APA might take to address racism and to rectify disparities in mental health care, medical care, and social equality.
Stay healthy,
Claire Zilber, MD, DFAPA
CPS President
Colorado Psychiatric Society COVID-19 Resource List
June 17, 2020
Updates |
|
CPS COVID-19 Resources for the General Public - CPS now has a webpage of COVID-19 Resources for the general public! It can be accessed from the CPS website homepage or at https://www.coloradopsychiatric.org/coronavirus. Resources are organized into the following categories: Key Resources; Self-care Resources; Colorado Specific Resources; Reopening and How to Stay Safe; Resources for Families and Children; Activities for Adults, Families and Children; Learn More about COVID-19; and Substance Use Resources. It is updated weekly so please share with your patients and anyone else who may find it helpful. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
June 10, 2020
Suicide Risk and Prevention During the Pandemic
Dear Colleagues,
The coronavirus pandemic is taking its toll on Americans' mental health, with more than 88,000 people developing anxiety or depression in May, according to a Mental Health America survey report. The per-day number of depression screenings was 394% higher and the per-day number of anxiety screenings was 370% higher in May than in January. Seventy-three percent of respondents with moderate-to-severe depression and 62% with anxiety also reported strong feelings of loneliness and isolation. Particularly hard-hit populations include LGBTQ individuals, caregivers, students, veterans and active duty military personnel, and those with chronic health conditions. Although the survey report doesn’t examine race/ethnicity, I would venture that communities of color, which are disproportionately impacted by the pandemic, also experience higher rates of depression and anxiety. More than 21,000 people considered killing themselves or harming themselves on at least 16 days during May. Nearly 12,000 had these thoughts almost daily. Between 40,000 and 50,000 Americans die by suicide every year, and in the month of May nearly half that many reported thinking about suicide. A crisis of suicide is looming, and psychiatrists must find ways to mitigate the factors that are accelerating suicide risk.
There was evidence of increased deaths by suicide during the 1918-19 influenza pandemic, and among the elderly in Hong Kong during 2003 SARS epidemic. This article in The Lancet identifies factors that increase suicide risk, including increased distress among people with preexisting mental health problems; increased rates of depression, anxiety and PTSD in previously mentally healthy individuals because of the stresses associated with social distancing; job loss and economic hardship; the stigma of having had COVID-19; and interrupted educational or occupational trajectories for teens and young adults. Furthermore, the increased prevalence of domestic violence as a result of shelter-at-home orders has been documented by the UN. Women, children and LGBTQ individuals are at increased risk of abuse, which may lead to suicide if the person feels trapped with no way out, or to homicide by the abusive person.
It’s too soon to know whether fears of increased deaths by suicide as a result of the pandemic will prove correct, but the CDC is analyzing information about excess mortality from all causes, including suicide, during the pandemic. The authors of this JAMA Viewpoint offer reasons for optimism as the rise of telehealth increases people’s access to treatment and a spirit of pulling together in adversity improves resilience.
On the other hand, a surge in firearms sales has been well documented, with sales up 71% nationally in April (1,797,910 guns sold) and up 85% in March (2,583,238 guns sold). Gun sales in Colorado were up more than 80% in April 2020 compared to the same time last year. Mind you, these are just the legal, registered sales.
We all know that suicide attempts by guns are the most likely to be lethal, with 82.5% of people who use a firearm sustaining a fatal injury. Although Colorado’s Red Flag Rule went into effect January 1, 2020, whereby family members or police can ask a judge to temporarily remove a person’s firearms if that person is deemed a danger to self or others, it’s not clear how or whether the unusual social restrictions of the pandemic will interfere with the law’s potential effectiveness. This article on preventing suicide by guns includes useful tips on storing guns outside the home, including with family members, a federally licensed firearms dealer, or a local police department. In Colorado, a friend may not take possession of a weapon for more than 72 hours unless a background check has been performed by the gun owner.
In my own experience with patients in the last ten weeks, I have noticed several trends. In patients with previously stable bipolar disorder who are also health care providers, the stress and sleep deprivation of adapting health care practices have precipitated manic or hypomanic episodes. Some patients with recurrent major depression or chronic anxiety disorders struggle with the disruption of their work and other routines. Perhaps most striking is the effect of the stress on patients who experienced abuse in childhood. For these patients, the masks recall episodes of suffocation; the adrenal hyperactivity recalls that state in childhood and seems to prompt regression to that traumatized state; the social isolation rekindles feelings of being left alone to fend for themselves. In my practice, this group of patients is struggling the most right now with thoughts about ending their lives.
I am now more likely to suggest ketamine in response to serious suicidal ideation, rather than inpatient admission. I’m mindful about which medications I’ll give in a 90-day supply, and which I won’t because of potential lethality in overdose. This article offers other pragmatic suggestions for actions psychiatrists can take now to forestall a suicide pandemic.
Psychiatrists may serve as beacons in the storm for our patients, our health care colleagues, and the person we encounter on the street who doesn’t even know we’re a psychiatrist. We may not know who is on the verge of despair, yet with each human encounter we have the opportunity to make a difference through a gentle demeanor, a kind gesture, a neighborly expression of concern, or an unexpected act of generosity. If we collectively strive to embody the ideal of the warm, patient, accepting psychiatrist in all our interactions, we add more grace to a world in dire need of courteous goodwill.
Stay healthy,
Claire Zilber, MD, DFAPA
CPS President
Colorado Psychiatric Society COVID-19 Resource List
June 10, 2020
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
June 3, 2020
Psychiatric Disorders and the Pandemic
Dear Colleagues,
Today’s column was supposed to be about the psychiatric effects of the pandemic, and it still will be. But first I must touch on current events. If you’re like me, you may have been settling into the new normal of practicing psychiatry, running a home and maintaining relationship connections during the pandemic. Recently I found myself thinking that I could live this way for the year or more that will be required: “I’ve got this.” Then Minneapolis police killed George Floyd and the country erupted. Sickened and enraged by yet another instance of police brutality towards a black man, protesters took to the streets. Unfortunately, perhaps exacerbated by the stress of the pandemic and its political and economic consequences, some of the protesters turned violent. Denver joined dozens of other cities with riots, curfews and the deployment of the national guard.
The murder of George Floyd has taken a psychological toll on many of us, but none more so than the black community. People of color, and black men in particular, live with the terror of police brutality in a way that I don’t. The riots also take a toll: from the sinus-inflaming smell of tear gas and pepper spray wafting over from downtown, to the noise of police helicopters circling overhead all night for the last five nights, to the swirl of emotions about the violence of both the rioters and police, to the outrage about how the White House is responding, all of this wears on me and everyone else I know. It adds to the urgency and gravity of the topic I’m covering today, which is the mental health effect of the pandemic on the general public, on people with preexisting mental illness and on the healthcare workforce.
A tidal wave of depression and anxiety is on its way, and we are already seeing the first of its surging swells. The UN has published a policy brief, COVID-19 and the Need for Action on Mental Health, highlighting the importance of mental health to a functioning society and concerns about the effects of the pandemic. This article from The Atlantic cites Colorado School of Public Health researcher Jennifer Leiferman, who found that Colorado residents have been nine times more likely to report poor mental health than during pre-pandemic times. Tom Insel of the NIMH discusses his concerns about the tsunami of mental illness about to hit us. Prescriptions for benzodiazepines rose 10% in March of 2020 compared to the same month in 2019, while antidepressant prescriptions rose at least 9%; as the stress of physical distancing, economic hardship and civil unrest continues, we can expect to see these rates soar, as discussed here. Although scientific studies have yet to be published about these impacts, we are already seeing case reports in the literature about COVID-19 related mental illness, such as this letter about new onset psychosis in a patient with no preexisting psychiatric history.
The impact of the pandemic on patients who already have psychiatric disorders cannot be overestimated. This letter in the Asian Journal of Psychiatry delineates concerns about exacerbation of anxiety disorders, depression, substance use disorders, and a host of other likely consequences of this “apocalyptic” pandemic on our patients. This case report describes an exacerbation of previously well-controlled OCD because of coronavirus contamination fears.
This literature review considers the effects of previous epidemics and pandemics on patients with chronic psychosis, which may help clinicians, researchers and policymakers address the needs of psychotic patients now. This detailed and thoughtful letter to the editor identifies challenges to optimizing psychiatric care during the pandemic, from changes in routines and social interaction, to increased vulnerability to infection and homelessness, to reduced use of treatment resources. Finally, this paper addresses the special adaptations to mental health treatment required for patients in detention.
The third population of special concern is the health care workforce, especially those on the frontline of COVID care. This survey of Italian healthcare providers revealed high rates of PTSD, depression, anxiety, and insomnia. Similar findings were found in a Chinese survey, which additionally identified that women, nurses and people at the epicenter of the pandemic were most likely to experience symptoms of distress. This interview with Eileen Barrett, MD, PhD, includes information about her experiences of physician distress among colleagues, how preexisting burnout among physicians complicates our adaptation to the additional burdens imposed by the pandemic, and suggestions for personal and institutional measures to ease the stress. This Perspective piece recommends three interventions at the institutional level and two at the national level to safeguard the health and wellbeing of health care providers responding to the pandemic.
In addition to national and institutional measures, which are critical, individual healthcare providers may take some steps to protect our wellbeing. We all know them: healthy diet, regular exercise, protecting sleep, emotional support from love ones, meditation or other mindfulness activities, psychotherapy and medications if indicated. Although I have a robust self-care regimen, I’ve noticed recently that my motivation to exercise hasn’t always been as perky as usual. This article offers advice about how to cope with this. (Washington Post, 5/12/20: Losing your motivation to exercise as the pandemic drags on? Here’s how to get it back.) PsychHub has developed a series of short videos on adaptation. Two of them are specifically targeted to HCPs, and may be helpful for individuals who struggle to manage their emotions. Although not specific to the pandemic, this thoughtful article on the power of physician self-care may help us break through the stoicism and stigma that prevent physicians from acknowledging our emotional struggles and seeking treatment for ourselves.
Governor Polis is aware that the pandemic is creating a mental health crisis. He has formed a Behavioral Health Task Force COVID-19 Special Assignment Committee to help address this. CPS member Kim Nordstrom has been appointed to the committee, and I hope she will share details from the draft report when it is available later in the summer.
Please scroll down to browse additional resources we’ve curated for you and for your patients this week.
Stay healthy,
Claire Zilber, MD, DFAPA
CPS President
Colorado Psychiatric Society COVID-19 Resource List
June 3, 2020
Updates |
|
CPS Members - Are you working on a resource that would be helpful to others during the pandemic? Are you speaking on a webinar or have you written an article on COVID-19? Please let us know by emailing [email protected] so we can help spread the word! |
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
May 27, 2020
CPS has a new President - Welcome, Dr. Zilber! Thank you to Dr. Westmoreland for her service and for writing the first 10 editorials for the CPS COVID-19 emails!
Substance Use Disorders and the Pandemic
Dear Colleagues,
Patricia Westmoreland, CPS’s immediate past president, set an outstanding example of leadership. Her weekly letters in our COVID-19 update were informative, friendly and encouraging. I intend to continue the weekly letters as long as people are reading them and finding them useful. Please remember to direct your patients to the CPS website to browse among the Resources for Patients available in each issue for links to self-care sites, taking care of children’s emotional needs at this stressful time, tips for social distancing as the regulations ease, and much more.
As the pandemic wears on into its third month in Colorado, we are moving out of the “acute response” phase and into the “settling in for a long haul” phase. The professional and lay press have been sounding alarms all along about the mental health consequences of the pandemic, so I want to take some time to address at least three specific topics in greater depth. In this letter, I discuss the effect of the pandemic on substance use disorders in three populations: the general public, people with preexisting substance use disorders, and health care providers. Next week, I’ll take a deeper look at mood and anxiety disorders during the pandemic in three similar population groups. The following week, barring a more pressing issue arising in the meantime, I’ll examine what we know about suicide in the pandemic.
When Governor Polis first announced the shut-down of all but essential services, marijuana dispensaries and liquor stores were to be closed. That lasted a few short hours. The outcry from the populace was deafening: we cannot get through this crisis without the ability to self-medicate our anxiety. I say this without a shred of judgment; I notice that, when I have a glass of wine now, I am tempted to pour a second glass more often, and I have reined in that impulse only because of an over-abundance of self-discipline (in other words, I’m a control freak). Apparently, I’m not alone. An editorial in the BMJ notes that alcohol sales in the UK were up 67% in mid-March, whereas grocery sales were up only 43%. The editorialists identify two populations of concern: those who already have an alcohol use disorder, and those who are on the brink of developing such a disorder as a result of bereavement, job insecurity or troubled relationships. According to the AP, alcohol sales in the US were up 55% in the week ending March 21. We would do well to ask repeatedly about alcohol, marijuana and other substance use in all our patients, even those for whom substance use has not been a problem.
For our patients in recovery, the pandemic has created a host of new stresses. Depending on the municipality, 12-step meetings have been closed for the last eight to ten weeks. The large one in my neighborhood only opened up last week, and under strict rules that limit attendance in order to comply with physical distancing regulations. A Buddhist alternative to AA, Recovery Dharma, has many online resources, including online meetings. Although it was published in 2009, I only recently became aware of Rami Shapiro’s interfaith book on the 12 steps, Recovery: The Sacred Art, which may appeal to people who associate AA with Christianity and/or who don’t feel comfortable with group settings. Seniors, who are at higher risk in the pandemic, are still advised to stay home, so in-person meetings aren’t available to them. Seniors with substance use disorders have additional health risks. Dr. Volkow discusses the effects of addiction on people’s risk for and susceptibility to infection with the novel coronavirus, challenges for maintaining recovery, and areas for future research in this short NIDA video. Dr. Volkow’s ideas are elaborated more fully in her Annals of Internal Medicine opinion.
There is concern that the pandemic may worsen the opiate crisis. Telehealth access and temporarily relaxed restrictions have enabled some patients to continue their treatment with buprenorphine, in effect removing a barrier to treatment. It remains to be seen whether some of these changes will become permanent policy. The variability among state regulations and the requirement of in-person dispensing means access to methadone has been more tenuous. Addiction recovery programs are finding creative ways to adapt to the pandemic, as summarized in this article.
A quick search on Google Scholar for papers related to substance use among health care providers responding to the pandemic came up empty. A search for papers on moral injury and emotional distress among healthcare workers in the pandemic yielded dozens of papers. I imagine that eventually the stress and moral injury may be reflected in an increase in physician impairment, but that data has yet to surface. In the meantime, please remember that CPHP’s COVID Care Line for Physicians is free and confidential.
Please scroll down to browse additional resources we’ve curated for you and for patients this week.
Stay healthy,
Claire Zilber, MD, DFAPA
CPS President
Colorado Psychiatric Society COVID-19 Resource List
May 27, 2020
Updates |
|
Register here for CPS Event (free CME) - PsychSummit: COVID-19, Climate Change and Mental Health is TODAY! Wednesday, May 27, 2020 at 11am MT (1pm ET) OR 6pm MT (8pm ET). Open to anyone.
This PsychSummit event will focus on climate change and mental health and open with comments on COVID-19 and climate change by David Pollack, MD. Then join our panel to discuss clinical examples and experiences, the role psychiatrists can play in advocacy and preparedness, and the ways we can best educate about the effects of climate change on mental health. The APA has designated this FREE live activity for a maximum of one AMA PRA Category 1 Credit ™.* More information and registration here. *Accreditation |
|
COVID-19, Physician Leadership, and the Urgency of the Moment in Medicine |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
May 20, 2020
PASSING THE TORCH – A REFLECTION OF LIFE LESSONS IN A TIME OF TRANSITION
Dear Colleagues,
It is with a mixture of sadness and anticipation that I write this last editorial as your President. I am honored to have served as President of the Colorado Psychiatric Society and I am also thrilled to pass the torch to Dr. Claire Zilber, who I hold in high esteem as a psychiatrist, an ethicist and a dear colleague. I can’t think of a person better equipped to provide compassionate and thoughtful leadership at this critical time in the history of medicine and psychiatry. As my farewell, I have put a short essay reflecting what I have learned as your leader during the pandemic that has changed all of our lives.
OUR TIME IS NOW
In her virtual address, AMA President Dr. Patrice Harris pointed out, “Physician leadership is critically important, and even more so now.” The AMA is currently advocating for loan forgiveness for frontline workers, urging Vice President Pence to exempt international medical graduates from immigration bans and requesting CMS make policy changes that improve the quality of care. The APA also supports these initiatives. At no time has it been more crucial that we psychiatrists stand up and count ourselves as members of the house of medicine and advocate for what is required to get us, our colleagues in other specialties and our patients through this pandemic. It is up to us to lead the charge in identifying and treating the mental health consequences of quarantine, isolation, loss and trauma. Mahatma Gandhi said: “First they ignore you, then they laugh at you, then they fight you, then you win.” Over the years, psychiatry has been dismissed by many, derided by some and challenged on a frequent basis. As I noted in my editorials on mental illness during the pandemic, psychiatrists are needed now more than ever. Several patients over the last few weeks admitted to inpatient psychiatry have told me how being isolated and having their lives turned upside has led to worsening of their symptoms. Our colleagues on the frontlines are suffering too. May is Mental Health Awareness month: now IS the time for us to lead the charge using our skill and knowledge to help our patients, our colleagues and ourselves.
WE ARE ALL IN THE SAME STORM (EVEN IF WE ARE IN DIFFERENT BOATS)
In addition to its many consequences, COVID 19 has highlighted the crisis of loneliness faced by many Americans. Loneliness, according to a New Yorker article, “is not just a feeling. It’s a biological warning signal that instructs us to seek out other human beings.” In addition to its psychological effect, loneliness takes a toll on us physiologically, inciting inflammation, wearing down our immune system making us more susceptible to illness. Dr. Sue Varma, founding medical director of the World Trade Center Mental Health Program at NYU, noted that while previous disasters have been finite, the uncertainty regarding the longevity of this pandemic is what makes it so hard to accept. According to a Time magazine article, a third of American adults feel lonely as a result of the pandemic. Who feels the most alone? Perhaps surprisingly it is not always those who live alone. Many individuals who are quarantined in a household where they get little time for self care also feel a sense of loneliness. Interestingly, elderly individuals appear to be less lonely once introduced to to social media, while Gen Xers may feel less lonely when they engage in activities away from social media. Clearly I am trending towards the former end of the spectrum: I enjoy scheduled FaceTime with friends and family, and waking (as I did one morning) to 50 “What’s App” text messages between my “international cousins,” the group of wily, wise and humor filled women alongside whom I was raised and now live in all corners of the earth. I will continue to set aside time to reach out to my family, my friends and my colleagues whose works of support and encouragement have guided me through my presidential year, especially the last few months.
“SOME DAYS I FEEL LIKE I AM MELTING:” PARENTING AND WORKING DURING A PANDEMIC
“Workenting” (working plus parenting): a word invented by me describing: a) completing my work as efficiently as possible so that I can devote a few uninterrupted hours to my children b) sitting on the sofa and watching a movie while working or c) the constant feeling that I am not devoting sufficient time to either pursuit. I previously described the multifaceted difficulties of parenting during this pandemic and they remain as such, especially for single parents – most of whom are single mothers. The New Yorker article I referred to is, I believe one of the best articles of the topic and is worth re-citing. A recent piece by Sheryl Sandberg, in which it is noted that women are working an average of 71 hrs per week on household and childcare related endeavors during the pandemic before they even begin to tackle the work for which they are paid, casts light on this problem. Sandberg advocates for companies to increase their flexibility with regard to work hours and eschew traditional metrics of job performance during the pandemic. As the uncertainty regarding school and college re-openings grows, and parents continue to struggle with managing their children (and keeping their jobs), having a support system is paramount, as is asking for help where we can, and marshaling our inner resources when we can’t. One such resources is humor – not only does laughing about the absurdity of lives improve our mood and strengthen our inner resources, but it also fosters a sense of togetherness. My favorite laugh of the week was this Washington Post article in which readers were invited to review their quarantine experiences as if they were reviewing a hotel. Tyrannical toddlers and lazy dog butlers aside, many of us are concerned about the psychological affects of the pandemic on our children – but there are some upsides of forced togetherness. In many homes (including mine) board games, neighborhood walks and bike rides, art projects, puzzles are more commonplace than ever before. It is important to cherish these moments especially at times where we feel that we are not doing enough, or being enough for our children and our partners. These are hard time, count your cherished moments and aspire to small successes every day.
“I AM BECAUSE MY LITTLE DOG KNOWS ME” (GERTRUDE STEIN)
My tenure as editorial writer of CPS COVID-19 Resources would not be complete if I didn’t mention the huge role that our dogs have played in helping me maintain my sanity over these last months. I am hardly alone in this regard. In “My co-anchor in pawing at the door” weather forecasters and newsreaders discuss adapting to the new normal of pets zoom-bombing their meetings in adorable fashion. Some of these adorable pets (kid Betty and cat) have gone viral (even if not in the COVID sense). There has also been an increase in pet fostering and adoption since the beginning of the COVD-19 pandemic (https://www.nytimes.com/2020/03/19/us/coronavirus-foster-pets.html and https://www.nytimes.com/2020/04/24/realestate/youre-quarantined-is-it-time-to-get-a-puppy.html). However in “America’s Pets can’t take quarantine anymore” we are cautioned to ensure that our animals get their space during our extended time at home. As the popular meme goes: “Dogs think we have given up our jobs to be home with them. Cats believe we have been fired for being the lousy humans they know we are.” Laughter aside, at no time has it been more clear to me how much we cherish the non-human loves in our life. Case in point my homicidal chihuahua mix. The warmth of his body, the smell of his fur and the sweet noises he makes as he falls asleep are an immediate panacea for moments of stress and anxiety. My partner (knowing how much I love this beast) gave me a dog DNA kit for my birthday. We anxiously await the results. His bet: part Chihuahua, Dachshund, possum and snake. I think he is thoroughbred Russian Toy dog (I learned that from my daughter’s dog breed book – she knows something about almost every breed). Wrigley’s genetic make-up is beyond the subject of this editorial. However, being invested in our dogs (and we have an additional two of known genotype), walking them together in the morning, curling up with them at night gives us a sense of shared purpose during these uncertain times.
THE WORLD CHANGED IN A MATTER OF MONTHS – BUT WE ARE IN CHARGE OF HOW WE RESPOND
During a weekend hike (this time thankfully sans rattlesnakes), my son and I reflected on how our world has changed in a few short months. Things that we had looked forward to – travel, school outings, skiing and visits with friends suddenly vanished. We also mourned the disappearance of events that would have marked milestones in our lives – for me, the CPS Spring Meeting where we would have hosted Dr. Patrice Harris here in Colorado; for my son, his elementary school commencement. Although we have much for which to be grateful, it is important to acknowledge these moments of grief. Former President Obama’s virtual commencement address encapsulated the feelings of disappointment felt by graduates, but was helpful in pointing out that events such as graduation ceremonies are transitory, but graduating into adulthood and having the power to make choices that reflect our values is what moving ahead is all about. In a previous editorial I wrote about the importance of resilience and how our sense of meaning and purpose, together with an ability to be creative in dealing with life’s curveballs, can shape our destiny. A recent New Yorker article expounds on how resilient people view the world differently, and discusses how resilience can be learned through dealing with the hard times in our lives.
I leave you with the wise words of Nelson Mandela, a giant of a man whose courage and resilience shaped a nation. “I never lose. I either win or I learn.” May we embrace the power of everything this pandemic has taught us as we move forward with fortitude and grace.
Patricia Westmoreland MD
President
Colorado Psychiatric Society COVID-19 Resource List
May 20, 2020
Updates |
|
This PsychSummit event will focus on climate change and mental health and open with comments on COVID-19 and climate change by David Pollack, MD.
Next, join our panel to discuss clinical examples and experiences, the role psychiatrists can play in advocacy and preparedness, and the ways we can best educate our patients and the public about the effects of climate change on mental health. The APA has designated this FREE live activity for a maximum of one AMA PRA Category 1 Credit ™.* More information and registration here. *Accreditation |
|
|
|
|
Telepsychiatry and the Coronavirus Disease 2019 Pandemic—Current and Future Outcomes of the Rapid Virtualization of Psychiatric Care by CPS Members Jay Shore and Chris Schneck and Matthew C. Mishkind, PhD |
|
Psychiatric Times Webinar - Telepsychiatry: Ready Your Practice for COVID and Beyond featuring CPS member Jay Shore - available on demand upon registration |
|
CDHS sponsored Channel 9News/Facebook Live event on Frontline Mental Healthcare workers- CPS Member Kim Nordstrom is a co-panelist with CCAPS member Dr. Christian Thurstone, Director for Behavioral Health (DHMC) and Renee Marquardt, Chief Medical Officer at CDHS. Scroll down to see event video. |
|
NEJM - Preventing a Parallel Pandemic — A National Strategy to Protect Clinicians’ Well-Being (5-13-20) |
|
COVID-19 Care Line for Physicians 720-810-9131 |
|
Washington Post - Losing your motivation to exercise as the pandemic drags on? Here’s how to get it back (5/12/20) |
|
APA Practice Guidance (updated 5-11-20) |
|
CMS Webinar - Social Determinants of Health and their Effects on COVID-19 Outcomes - Friday, May 29, 12-1 p.m. Registration and full accreditation statement here. |
|
APA, Inc - Returning to Work During COVID-19 Recovery (download) |
|
Redeployment to COVID-19 Care Is Like Treading Water but Deeply Gratifying(5-11-20) |
|
|
Consider these ways to reframe COVID-19 to speak with youth and manage stress and anxiety - short article by CCAPS member Chris Thurstone |
|
The New Yorker - Advice for the workplace - Atul Gawande explains how businesses can minimize the virus’s spread when they reopen by copying what hospitals are doing with their employees. |
|
Vanity Fair: If 80% of Americans Wore Masks, COVID-19 Infections Would Plummet, New Study Says |
|
Washington Post - Your questions, answered - “My father was a healthy, 96-year-old senior with a robust social life at his assisted-living home. Now, after 60 days of total isolation, he is a depressed, run-down, lonely shell of his former self with no quality of life and no end in sight. Is this really the best way to handle this pandemic in our senior communities? How can people help?”— Lynn (5/12/20) |
|
Washington Post - Losing your motivation to exercise as the pandemic drags on? Here’s how to get it back (5/12/20) |
|
Headspace - Headspace Plus is now FREE for every unemployed person in the US. An app for users to discover meditation and mindfulness tools to help feel less stressed, more resilient, and kinder to yourself. |
|
The Centers for Disease Control and Prevention (CDC) has released six "decision trees" to help businesses, workplaces, schools, camps, transit, and other communities decide whether it is safe to reopen |
Key Resources |
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
May 13, 2020
COVID-19 as a teachable moment in uncertain times
Dear Colleagues,
“In a time of fear and uncertainty the best thing to have is a protocol,” wrote Lisa Rosebaum MD in an article in New England Journal of Medicine Perspectives. Of all the characteristics that people recognize me for, I would say that “takes on new challenges” is fairly well known. Not as widely known, perhaps, is the angst that follows the initial surge of enthusiasm. Was this a good decision? Do I have what it takes to handle this new challenge? What are the pitfalls? Such were the threads of my post-decision thought process after I decided to accept the job as psychiatry residency training director for a newly accredited program in the Denver area. I had a vision as to how I might prepare for stepping into this role, and what it would be like to do so, and what issues I would need to address at the outset – i.e. the beginning stages of developing a protocol. Then COVID came along. Like everyone else, many of my plans for the upcoming months turned to dust. Aside from the constants of my home and loved ones, I was in that strange no man’s land that comes with exiting one job and beginning another. All of this transpired in a rapidly changing world. Adjustment, as we psychiatrists know, takes time. Although I am only now adjusting to a new normal, I will soon have the challenge of shepherding residents through a rough terrain with no identifiable roadmap. To say that I am thrilled, excited, honored and at the same time apprehensive is to only begin to fathom the myriad of emotions I feel – and the enormity of the challenge that lies ahead.
What is known about residency training during the COVID pandemic? What has been expected from residents and how have they responded to this massive disruption in their journey? In “We signed up for this! – Student and Trainee Responses during the COVID-19 pandemic," Drs. Gallagher and Schleyer discussed the role of medical students and trainees (residents and fellows) during the emerging days of COVID-19, and how to balance clinical and educational objectives with the safety and wellbeing of these students and trainees. To learn more about how their students and trainees were affected, they conducted an anonymous survey of 316 students and trainees. Respondents’ anxieties were amplified the closer they were to the frontlines and their safety concerns were complicated by concerns about transmitting infection to their loved ones (see Am I Part of the Cure or Am I Part of the Disease? Keeping coronavirus out when a doctor comes home). Students and trainees also reported moral distress at seeing patients dying alone, feeling they themselves could not be useful and many were beset by practical challenges such as childcare. Interestingly (but not surprisingly), despite their anxieties, students and trainees frequently expressed a desire to help, often volunteering for extra duties – an admirable esprit de corps.
When residents voluntarily go the extra yard, as training directors we should be right there with them. What can we do to help residents through these unprecedented times? Although not psychiatry specific, ACGME reminds us of the importance of balancing the increased demands for clinical care with training requirements, ensuring we adhere to resident work hours, as well as adequate instruction in use of PPE and other infection control measures. A brief article from the American Association of Directors of Psychiatric Residency Training (AADPRT) reminds us to advocate for our residents, express gratitude for their working under extraordinary circumstances, and monitor their wellbeing. Communicating frequently with residents as well as maintaining structure were also seen as key. Authors of a letter to Psychiatry Research entitled “Disrupting the Disruption: using digital tools to support psychiatry residency training in Singapore during the COVID-1 pandemic” noted that the last event that significantly disrupted residency training (i.e. the SARS epidemic in 2003) was contextually different in several aspects, one of the most notable being technology. At that time, videoconferencing capabilities were not as advanced as they are currently are. Despite constraints on social gatherings, residents can continue to discuss cases with their supervisors and supervisors can assess the skills of their residents. The authors noted that in their institution, participation rates in clinical case presentations and discussions have been good, and the expansion of the availability of didactic lectures to various sites (which was not as well developed before the pandemic) has proved useful. Videoconference modalities can also be used to assess resident wellbeing (remembering that loss of social connectedness is a major contribution to physician burnout) as well as to update residents on schedule and logistical changes as they occur. However, the letter cautions that we must also remember the difficulties that could be encountered by trainees, many of whom are still learning the communication skills inherent to interviewing patients, which is made doubly difficult by having the use of telemedicine – or the use of videoconference in supervision where subtle nonverbal clues between supervisor and supervisee’ may be missed or misinterpreted. Teamwork can thus become fractured, and the opportunity to learn from mistakes (i.e. teachable moments) is therefore missed. The work of Harvard Business School’s Amy Edmonton (as noted in an Editorial on teamwork) teaches us that, while teams who work closely together don’t necessarily commit more errors, they are just more likely to learn from them.
The authors of “We signed up for this” denoted COVID-19 as a teachable moment, stating that the “chaos and uncertainty” engendered by this pandemic “demand an unyielding focus on core medical principles and consistent modeling of professionalism, altruism, quality and safety.” How do we, as leaders, expand on these objectives in a clear, consistent and reassuring manner, while at the same time dealing with our own fears and uncertainties? To quote Mark Whatney, fictional astronaut in The Martian (one of my all-time favorite movies): “You just begin. You do the math. You solve one problem then you solve the next problem then the next…And if you solve enough problems, you get to come home.” I plan to teach my residents, in the coming weeks and months: residency is by and large about learning to confront uncertainty, ask for help, learn from your mistakes, improve the lives of your patients - and solve problems. It is about growing intellectually as well as emotionally and learning from teachers who have had as steep a learning curve as any in the past few months. According to Buddha, “Your worst enemy is your best teacher.” And from COVID-19 have come both.
Patricia Westmoreland MD
President
Colorado Psychiatric Society COVID-19 Resource List
May 13, 2020
Updates |
|
REGISTER HERE! Non-members welcome! |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
May 6, 2020
A PANDEMIC IS NOT A TIME FOR PERFECT
Dear Colleagues,
Last week I wrote about “okay parenting.” Not a distinguished title or aspiration for a parent but one that I felt was befitting for a time when managing (rather than excelling) is the order of the day. I was reminded of this during a recent attempted hike in Boulder. At the foot of the trail a large sign warned: “Be aware: rattlesnakes have recently been seen on the trail. Be careful when hiking trails in this area. Rattlesnakes are common this time of the year.” About 10 yards further up the trail we were treated to the sight of a large ominous rattler who had recently recently consumed something of sizable proportions. I about died. I am deathly afraid of snakes – especially the venomous ones. I tried to take a few steps forward but found that I could not go on. “Where’s your persistence Mom?,” came the response from my bold 11 year old. “Sometimes,” I said, “its good to know when to call it quits.”
According to those who are seasoned at hiking rattlesnake country I made a good choice. But giving up is not in my nature and I had a tough time with ending a hike that had barely started. That said, there are times when our sense of perfection and the need to have everything turn out as planned is self defeating at best and (in the case of the rattlesnake) potentially lethal.
During the beginning stages of our quarantine, an article in the New York Times lamented, “the internet wants you to believe you aren’t doing enough with all that extra time you now have.” The author of the article noted that, as the Coronavirus has kept us home, many people are feeling pressured to organize every room in their homes, become expert chefs, write a book or get in shape. The article goes on to state that the urge to over-achieve (even during a pandemic) “reflects America’s always-on work culture.” The idea that we have the extra time during lockdown to achieve a myriad of things (and the extra energy to realize those goals) is a fantasy. Balancing work and family responsibilities, all of which often occur under the same roof, is enough in and of itself.
An article in Bloomberg Businessweek indicated, now is not the time to be perfect. The drive to be perfect may also be be lethal to physicians. In a New York Times op-ed memorializing Dr. Lorna Breen, the New York emergency room physician who committed suicide after both treating COVID-19 patients and becoming ill with the virus herself, author Jennifer Senior wrote “physicians are perfectionists who suffer in silence.” She noted that we are trained to project confidence and move forward, and seeing ourselves as vulnerable is antithetical to our self concept. Ms. Senior wrote that, while we cannot extrapolate too much from Breen’s case, it should be noted that she was the second known American health care worker to die from suicide in this pandemic – and neither Dr. Breen nor the 24 year old Staten Island paramedic who died as a result of suicide had a known history of depression or suicidal ideation. Being driven and identifying as a high-achiever who wants to solve problems has become inordinately difficult in the face of a virus that defies our previously held notions that, when faced with an illness, physicians are able to manage that illness treat it and the patient most often gets better.
The feelings of helplessness described by ER physicians in treating COVID-19 patients is not new to us as psychiatrists. Psychiatric illness is much less well understood than other illnesses – including infectious diseases. There are no metrics that tell us with great certainty whether our patients are going to kill themselves or others. We can’t verify our patient’s affective symptoms though laboratory tests or imaging modalities. While there have been major improvements over the years, our medications are not always effective and, despite the advent of genetic testing, we don’t know which medication to try first. While that does not mean we are necessarily less perfectionistic than our colleagues in other specialties, and although we have not experienced death in the numbers seen by our ER colleagues during the last few months, we are accustomed to a greater degree of uncertainty which may help us navigate this crisis both personally and professionally.
A New England Journal of Medicine article entitled “Physician burnout, interrupted,” promotes the idea that operating in a new and imperfect world may actually invigorate medicine. Drs. Hartzbrand and Groopman write that, during these times of uncertainty, a sense of altruism towards the medical field has “unexpectedly catalyzed the restoration” of some of the elements that had traditionally led to burnout: lack of autonomy, competency measured mostly by meaningless metrics, and lack of relatedness.
While there has been some gain in autonomy and the relaxation of rules governing how we practice medicine, psychiatrists should probably be most cognizant of the relatedness piece. Not because we don’t relate, but because we may relate too much. Wading in the uncertain quagmire of human emotions is a difficult experience especially during one of the few times in history when we are faced with the same nemesis as our patients, and this may be where our professional sense of perfection is challenged. In “Therapists and patients find common ground: virus-fueled anxiety,” Sarah Maslin Nir notes the parallel processes of therapist and patient during COVID-19. She writes about a psychiatrist who specializes in women’s health who stated that the effect of absorbing the same worries as her patients made her collapse into bed at the end of the day. The psychiatrist, who said she had formerly experienced her patients’ worries as separate from her own, felt the same worries encroaching into her emotional life. However, she knew weathering the storm meant having goals that were more modest than she might have had in times past.
How do I get through that storm? Winston Churchill said, “If you are going through hell, keep going.”For me that means getting my job done, dealing with my loved ones, checking in on friends, reading my novels and being even more attentive to my dogs than they can tolerate (more on that later). I have no compulsion to forge every possible path (especially those with rattlesnakes). At least not today. As web designer Izey Victoria Odiase said, “don’t aim for perfect. Aim for better than yesterday.”
Patricia Westmoreland MD
President
Colorado Psychiatric Society COVID-19 Resource List
May 6, 2020
Updates |
|
Saturday, May 16, 2020 5pm MT REGISTER HERE! Non-members welcome! Patrice A. Harris, MD, MA, president of the American Medical Association (AMA), will discuss the AMA’s multi-faceted response to the COVID-19 pandemic, including specific ways of responding to the mental health needs of physicians and the public during this time of crisis. The evening will begin with an opening session featuring an interview between New York Times Op-Editor Dr. Richard A. Friedman and comedian Gary Gulman of HBO's The Great Depresh.      |
|
CMS has updated the telehealth list with those codes that can be done via audio only. On April 30, 2020, CMS issued a new ruling permitting audio only telephone care for the following psychiatry codes: 90785, 90791, 90792, 90832, 90833, 90834, 90836, 90837, 90838, 90839, 90840, 90845, 90846, 90847, 90853. CMS also announced they will be increasing payments for audio-only telephone visits (99441, 99442, 99443) between Medicare beneficiaries and their physicians to match payments for similar office and outpatient visits. The changes to billing for audio only are retroactive to March 1, 2020. The updates are for patients that cannot do the video piece; members can still bill as they always have if they do both audio and video. 99441 (5-10 min; $46) 99442 (11-20 min, $76) 99443 (21-30 min; $110) Since the add-on psychotherapy codes, 90833, 90836, and 90838 have been permitted for just audio, the APA believes CMS is recognizing it will be acceptable to bill for an E/M with one of these codes even when only audio is available using the point of service for where the encounter would have taken place were it not for the public health emergency, and the modifier 95 is to be used to indicate the care was provided via telemedicine. The APA is waiting for confirmation from CMS that this is the case and will provide updates here. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Resources for Patients
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
April 29, 2020
Okay To Be Good Enough: Parenting In The Age Of Covid-19
Dear Colleagues,
I woke up with the burglar alarm blaring and my phone ringing. It was 2am and I was barely awake but conscious enough to know that I needed to check things out. Armed with cellphone (ADT operator in tow) and a small but potentially lethal canine, I made my way downstairs. The door that has given trouble previously was shut tightly. Could it have been open and closed in haste by a fleeing intruder? Was there someone in the house? Although nothing seemed out of place I agreed to have the operator notify police. “Do you have any weapons in the house Mam?,” asked the officer “Not unless you count an 8lb chihuahua,” I responded. A member of the Denver Police Department (complete with face mask) dutifully inspected the premises and left, my son went back to sleep. Our labradoodle slept through the entire event, befitting her reputation as a great family dog, but lousy watch dog. Pint-sized killer dog and I remained vigilant for several hours until we fell into a fitful slumber.
Last night’s alarm episode closely mimics the new reality that I, as well as others, now face on a daily basis. COVID-19 has disrupted our lives. We have had to wake up quickly and respond. We are fearful. Our immediate instinct is to protect our families. We try to do our best. We feel off-kilter. We try to find humor in our up-ended lives. Parenting during a pandemic takes these feelings to a whole new level. The complexities of home schooling, keeping our children occupied when they have completed their schoolwork and helping them navigate this strange new world seem endless. For those working from home, as meme doing its rounds on Facebook instructs us, “You are not working from home; you are at your home during a crisis trying to work…I think it’s an important distinction worth emphasizing.”
“We are all stressed out” is the title of a USA Today article discussing the feelings of experiences by both parents and children during this pandemic. Disruption in their normal routines, anxiety over outside threats and diminished social interactions may lead to anxiety and depression in children. The USA Today article indicated that over half of the 562 parents surveyed in a University of Michigan study noted that self-isolating and financial worries were hampering their abilities as parents. Over 60% admitted to shouting and screaming at least once since being secluded in their homes, and one in six admitted to spanking their children. The study’s lead author cited concern that, with continued absence from school, there will be fewer adults to whom these children can report the abuse. The American Psychological Association has also expressed concern that the incidence of child abuse (as well as spousal abuse) will increase during this pandemic as it has with prior disasters such as hurricanes. Factors that increase the risk of violence are reduced access to resources, increased stress related to job loss or finances, and disconnection. Sadly, sex abuse hotlines have experienced a surge in calls as victims and their abusers are housebound together.
Caught between Scylla and Charybdis, those who are single parents have already had to choose between having a partner who is unhelpful at best (downright violent at worst) and the uncertainties of going it alone. COVID-19 has intensified that burden and added some strange legal twists. “How are parents supposed to deal with joint custody now?” asks an article in The Atlantic. According to a New York Times article, child custody is now the “new battle” for frontline workers. The article details the case of a New Jersey internist whose husband presented her with a court order demanding sole custody of their daughters. A google search indicates such a situation is not uncommon: frontline workers feel they should not be punished for their role in helping others while their counterparts contend that that they are risking their children’s lives. With courts either having no roadmap for dealing with the current status quo, or are just not open at all, warring exes may feel entitled to re-write their custody agreements sans judicial oversight.
“Some days I feel like I am melting,” reads the title of an April 21st New Yorker article. While the burdens of COVID-19 are hurting all parents, they fall disproportionately on single mothers. Author Emily Bobrow noted that almost a quarter of children in the US live with a single parent (a higher percentage than anywhere else in the world) and most of these single parents are single mothers. In addition, it is the industries that employ large numbers of women (childcare, housekeeping, hospitality, retail and travel) that have been affected the most by COVID-19 related restrictions. They also frequently work in jobs that expose them to contagion (nursing) and which lack protections such as paid sick leave (Time Magazine article). For women who have been able to keep their jobs, one in three jobs held by women are categorized as essential: but how do these women do their work as well as be the chef and the teacher and find time for self care? In contrast to the “silver linings” of the pandemic that has been touted for traditional nuclear families e.g. having a husband (or wife) who can now pitch in and assist with schoolwork and household tasks, social distancing has rendered single parents more alone than ever. Social media intensifies feelings of guilt and failure (also see Why mothers are bearing such a huge mental load during coronavirus pandemic). It is hard to feel good about one’s own goal of surviving the day when faced with everyone else’s perfect family pictures on Facebook, even though we may know that the pictures likely tell only half of the story.
“Its okay to be a different kind of parent during the pandemic,” (What Losing My Husband Taught Me About Pandemic Parenting) wrote Mary Katharine Hamm, who was seven months pregnant and raising a two-year-old when her husband died in a cycling accident. In a scene reminiscent of Joan Didion’s book “The Year of Magical Thinking”, in which Ms. Didion’s husband dies at the dinner table (and her daughter dies shortly thereafter), Ms. Hamm writes, “You’re probably feeling like you’re seated at that table now. The Coronavirus is serving up a rare and tragic mix of grief, drastic life changes and economic stress.”
Ms. Hamm noted that, “When something outside your control changes your life, it’s what you do with what you can control that really shapes your children.” She writes that believing in one’s abilities and practicing those abilities with a view to “small wins” is key. Tradeoffs and perspective are also important. I think about this a lot as I try to juggle work and kids: time to play ping pong with my exuberant son or watch a dog movie with my animal-crazy daughter are no less important than a home cooked meal (especially one cooked by me). And nobody will die if the laundry is not neatly folded and put away as soon as it exits the dryer. It was far more beneficial both intellectually and for my feelings of connectedness to participate in the APA assembly than be enslaved by laundry.
Lowering our expectations during this pandemic might actually be beneficial (CPR News article (download)), and parents may struggle more if they set too high a bar for keeping their children engaged while trying to manage their own new reality. UC Anschutz Child psychiatrist Dr. Amy Lopez noted that its okay for children to be bored and “their boredom is not your problem.” Those of us who grew up in the 70’s would agree with Dr. Lopez’s contention that working parents today spend more hands on time with their children than did stay at home mothers in the 70’s, an era when “go play outside and play” meant just that, and our boredom engendered our creativity.
While the list of resources I have enclosed is certainly not exhaustive, the “parenting during COVID-19” articles I selected (see below) share several common themes: navigating uncertainty, picking our battles, establishing routines, encouraging virtual social interaction, making time for physical activity, validating our children’s feelings and taking care of our own mental health. The latter is more important than we have been taught to believe: there is a difference between self-indulgence and self care. The tragic death by suicide of physician Dr. Lorna Breen, who had both survived COVID-19 and treated Coronavirus patients is a painful reminder that we are all vulnerable. While we do not know why Dr. Breen took her own life, her death is indicative of the wave of mental anguish arising from the pandemic and its impact on our daily lives. Let’s start small, be thankful for what we did get done today (even if it wasn’t perfect) and teach our children and our patients to strive for the same goals.
Patricia Westmoreland MD
President
Parenting During Covid-19 Articles
How To Care For Your Kids' Mental Health During The COVID-19 Pandemic (download)
Parenting amid COVID-19_ Expert tips on how to help kids at home (download)
4 Life Skills Parents Can Teach Kids Amid The Coronavirus Pandemic
Colorado Psychiatric Society COVID-19 Resource List
April 29, 2020
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
April 22, 2020
SAVING OUR COLLEAGUES, SAVING OURSELVES
Dear Colleagues,
After rounds on Saturday morning, I stood on my partner’s deck, a mandatory six feet apart, waiting for the Thunderbirds to fly over. I joined a Facebook watch party. I started my own Facebook watch party. I was overwhelmed by the response: watching the Thunderbirds fly over Denver with childhood friends, medical school compatriots and my Denver friends and colleagues was an experience unlike no other. Those who know me have described me as hard-charging, matter of fact, self deprecating and not usually given to displays of public emotion. The appearance of the Thunderbirds turned me into into a tear- soaked mess. Turns out I was not alone. In reference to the Thunderbirds, a child psychiatrist friend wrote, “I’ve made an unintentional habit of breaking down in some form of cathartic tears every time I’ve gone for a run during this lockdown and I thought I was going to make it through today’s run and then this happened…We are all dealing with many emotions today.”
In a stirring tribute to her physician mother (youtube video), a young woman composed a melody entitled “Doctors are the Heroes of the Day.” Her powerful lyrics eloquently praise our sense of duty in getting up every morning and “running towards the fight.” She reflects that, although we do not have the “super-strengths” of traditional super-heroes, doctors inspire hope in others. In so stating, she captures the essence of Pascal’s statement: “Small minds are concerned with the extraordinary, great minds with the ordinary.”
COVID -19 has become the struggle of the ordinary: doctors, nurse and other healthcare workers have been subjected to its daily ravages en masse. What is it like to stare down one’s own fears on a daily basis and what is the cost of doing so day in and day out? I suspect that we are going to find out in the not too distant future. Once the mode of operating at critical capacity begins to slow down, our frontline healthcare workers will begin to take a true accounting of what they have witnessed and endured. How they fare will be determined in large part by how proficient we become at acknowledging their heroism as well as their suffering, and helping them find a way through their pain.
In one of the first published articles detailing the mental health effects of caring for patients with COVID-19, Lai et al described the results of a cross sectional study of 1257 healthcare workers in 34 hospitals caring for individuals with COVID-19. They found that over 70% of healthcare workers reported feeling distressed, 50% experienced depression, over 40% experienced anxiety and almost 35% experienced insomnia. The most detrimental effects were noted in frontline workers, nurses, females, and hospitals at the epicenter of the outbreak. The authors of the study recommended the immediate implementation of special interventions to promote mental health in these workers.
In a CNN opinion piece living apart from spouse and children, frustration over work conditions, feelings of helplessness, frustration at lack of resources, the trauma of multiple deaths, seeing colleagues fall ill and fear of their own death were identified as contributing to the distress experienced by healthcare workers. A Time Magazine article (add link) added several more areas of concern: the fear experienced by physicians who are afraid not only of becoming ill but of infecting their families, the exhaustion of working long hours with no end in sight, and feelings of deep sadness at seeing patients die. The death of such patients, without their loved ones at their side incurs an even greater burden for healthcare workers who take on the role of passing emotionally laden farewells from family members to patients. An ICU nurse interviewed for that article noted, “We’re all affected. To say that we’re not would be a lie.”
“I’m an ER doctor in New York. None of us will ever be the same” details the struggle of an ER physician in adapting to the rapidly changing and horrifying status quo of fighting COVID-19. She discusses the immense burden on physicians of being accused of “playing God” in allocating resources, how to best distribute risk amongst healthcare workers and the perils of incubating patients without face shields because none were available. Dr. Ouyang noted that mental health professionals “especially those who treat combat veterans” worry that doctors will sustain moral injury from having to allocate medical equipment and care. However, she noted that what will probably cause the most moral injury is seeing people die over and over again; “that I am the last person they see before they die – not their families – and that I won’t remember them at all because there will be a hundred more just like them. That it will become routine.” Dr. Ouyang also writes that she has never felt less useful as a doctor but “the one thing I can do - what I think will matter most, in the end, is to just be a person first for those patients and their families.”
How can we, as psychiatrists, support our colleagues in being “a person first” given the desperateness of the situation in which they find themselves? Our President-elect, Claire Zilber, reminded me that this week marks the birthday of one of the founders of Psychiatry, Dr. Philippe Pinel. Dr. Pinel, born in 1745, became the chief physician at a Paris insane asylum, by all accounts a horrific place where patients were chained to the walls and people could pay a fee to see them. Pinel put a stop to these practices. Instead of believing that the insane were possessed by demons, he started treating patients by talking to them about their problems on a regular basis, which paved the way for modern psychotherapeutic practice.
Jump ahead almost 300 years and the time to employ those skills is upon us. Our colleagues who have witnessed so much need us as never before. It is our duty to listen as they voice their inner heartbreak, and our calling to support them as they re-emerge into a world that can barely comprehend the horrors of their daily struggles. According to the Time magazine article, healthcare workers have found their most meaningful relief through the support of their families, friends, and colleagues. Hospitals have also come to the aid of their workers. Mount Sinai, for example, set out to provide assistance based on Maslow’s hierarchy of needs – assisting staff with the most basic needs such as childcare, cab fare (when taking the subway has become too perilous), as well as counseling and psychosocial support (see AMA report). Helplines have been set up around the country to assist with the mental health crises of healthcare workers even though this is not likely to come fully into focus until the immediate needs engendered by the pandemic have ebbed. We need to continue cheering our fellow healthcare workers as they do (with nightly applause) in New York and Thunderbirds in Colorado.
As my child psychiatry colleague wrote: “And to the Air Force Thunderbirds, you’re welcome. I am honored to be a physician and proud to be doing the work that I do.” Let’s extend that pride to helping our colleagues through a time like no other.
Thank you to Hannah and Dan Hyatt, Dr. Barbara Kessel and CPS President-elect Dr. Claire Zilber for their contributions to this editorial
Patricia Westmoreland MD
President
Colorado Psychiatric Society COVID-19 Resource List
April 22, 2020
Updates |
|
PsychSummit is a partnership between the Colorado Psychiatric Society and the New York County Psychiatric Society. From the beginning it has been a VIRTUAL INTERACTIVE conference designed to bring together psychiatrists from across the country (and beyond) to discuss some of the most pressing issues the profession faces. We held a last-minute special COVID-19 edition on Sunday April 19th and are thrilled that almost 670 people registered in less than a week! |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Key Resources |
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
April 15, 2020
Dear Colleagues,
“I treasure our walks.” The intense emotion behind this statement stopped me in my tracks. While walking our dogs has always been a favorite part of our time together, it never entered my mind that it would be the only time that we could safely spend together, and any misstep in our social distance could endanger the man I love. Such is life under the regime of COVID-19. We demonstrate our love by physically separating, despite having the technology to connect virtually. However, the privilege of 21st century technology is not without detriment. The more technologically connected we are, the more we are bombarded by news feeds (each with more dire predictions than the one that preceded it). The more we see pictures of friends and family on FaceBook and other social media platforms, the more we are reminded of the physical connection that we miss. I suspect that all of us have moments of petulant rage and self pity as we survey our lives and take stock of what we think we have lost. Is this the next phase of COVID-19 and will it ultimately be more damaging to humanity than the one that preceded it? What is the nature of that damage to ourselves and our patients and how do we mitigate it? CPS and NYCPS are hosting a free event this Sunday evening for psychiatrists across the country to learn from each other, share experiences, brainstorm solutions--and raise conversation topics for the next phase of the pandemic. We hope you can join us.
In a news article entitled “Mental illness will be ‘next wave’ of the COVID-19 pandemic” a reporter for a Canadian news channel noted that continued physical distancing will take a toll on our mental health. Quoting a public health expert who studied the psychological effects of the SARS epidemic, journalist Eva Ugeun-Csegne noted that the isolation - as well as the uncertainty about how long it may last - all contribute to increased anxiety, along with depression and increased substance use. The stress of caring for and home-schooling children, financial strain and unemployment adds to the burden.
South African psychiatrist Dr. Stoffel Grobler termed these stressors “burn-in,” likening them to cabin-fever – i.e. the psychological response to being cooped up in confined spaces during winter. Dr. Grobler wrote that the feelings of restlessness, depression, irritability, and decreased motivation all sounded “very familiar considering how people have been reacting to the lockdown measures.” He added, “In many countries including South Africa, the rate of domestic violence has also increased. Glaring reminders that we are all suffering psychologically.” According to Dr. Grobler “it seems logical that the prevalence of mental illness is about to increase exponentially” (SAMA Insider, May 2020, in press).
Dr. Grobler in not alone in his concerns. In their article “Mental Health and the COVID-19 pandemic” published yesterday in the New England Journal of Medicine, Drs. Pfefferbaum and North wrote that the effects of public health emergencies “translate into a range of emotional reactions” (such as distress or psychiatric conditions) and unhealthy behaviors (e.g. substance use). In enumerating the emotions which result from being quarantined, they described the symptoms enumerated in Dr. Grobler’s “burn-in” hypothesis down to the last word. They also sounded the alarm that individuals with pre-existing psychiatric problems are at greatest risk for adverse psychosocial outcomes. This sentiment was echoed by APA President elect, Dr. Jeffrey Geller, in a recent Psychiatric News article in which he and his co-author noted, “for many individuals with mental illness, being alone is a terrible burden, far beyond that experienced by others."
Sometimes that burden is impossible to bear. In their article “Suicide mortality and Coronovirus disease 2019 – a perfect storm,” published last week in JAMA, Drs. Reger, Stanley and Joiner enumerated factors inherent to this pandemic that increase the risk for suicide. These factors are economic difficulties, isolation from family, decreased access to community and religious support, increased firearm sales, increased substance use and most unfortunately the coinciding of the peak season for suicide (late spring/early summer) with the predicted peak of COVID-19 infections. On a more positive note, the authors noted that there could be a “silver lining” to our current status quo. They hypothesized that the reason for a decline in the rate of suicide after past national disasters is a so-called pulling together effect where a community whose members are all subject to a detrimental event come together to support one another. In another recent JAMA article, The Mental Health Consequences of COVID-19 and Physical Distancing: The Need for Prevention and Early Intervention, the authors outline 3 steps, taken now, that can help prepare for the inevitable increase in mental health conditions. To those of us who are psychiatrists, our job is to cement that effort for our patients who cannot do this on their own. As psychiatrists we are obligated to help our patients deal with this pandemic, leading by example even on days when we are beset by our own pain and limitations.”
Ronald Reagan stated, “To sit back hoping that someday, someway, someone will make things right is to go on feeding the crocodile hoping he will eat you last, but eat you he will.” Mental health must not be given the last thought. A recent article in Forbes magazine summarized the strategies used by world leaders whose countries are thought to have had the best response to COVID-19. A realization of the seriousness of the problem, decisiveness, a willingness to embrace technology and empathy were all cited as characteristics of these progressive world leaders.
Is it a coincidence that all of these leader are female? Regardless, we as psychiatrists would do well to embody their forthright manner in dealing with COVID-19. We can do this! A foray into the travails of mental illness is a journey into the land of the uncertainty, and we have been trained to deal with it head on. Self-selected by our choice to become psychiatrists, we are usually adept at intuiting the feelings of our fellow human beings and empathizing with their struggles. We also need to be reminded that we have these qualities.
“I miss you,” I told my partner as we marched six feet apart through the bitter cold day. “Why?” Came his reply. “I am right here.”
Patricia Westmoreland MD
President
Colorado Psychiatric Society COVID-19 Resource List
April 15, 2020
Updates |
|
Dedicated discussion rooms will include:
This event is FREE for all psychiatrists and trainees! Register now at: www.psychsummit.org
|
|
|
Contingency Planning for a Pandemic by Claire Zilber, MD, DFAPA (download) |
|
COVID-19 Testing for healthcare workers CDPHE is currently partnering with Kaiser Permanente to help provide COVID-19 testing to symptomatic health care workers and first responders, including those who are not Kaiser members, who do not have access to testing through their employer. Testing is available at eight locations between Loveland and Pueblo. To schedule an appointment, contact CDPHE at 303-692-2700 and ask to speak with a clinical consultant about Kaiser testing. |
|
Self-Care Advice for Health-Care Providers During COVID-19 by CPS’ Rachel Davis, MD; CCAPS’ Steve Berkowitz, MD and Helen Coons, PhD |
|
Health First CO Medication Prior Authorization Deferments - 4/7/2020 (download) Highlights: Prior Authorization (PA) requirements for Health First Colorado (Colorado's Medicaid Program) members on all medications for which there is an existing 12-month PA approval in place are being deferred. Each PA may be extended one time for 90 days. These extensions will be handled on a case-by-case basis by the Magellan Rx Management Pharmacy Call Center (1-800-424-5725 for a one-time PA deferment). New PAs and existing PA approvals that are less than 12 months are not eligible for deferment. |
|
Telepsychiatry in the age of COVID-19 with CPS Member Dr. Jay Shore (podcast) - Dr. Jay H. Shore discusses telepsychiatry in a regulatory environment that is quickly changing because of the physical distancing forced by the COVID-19 pandemic |
|
Register for the Physicians' town hall on COVID-19: Wednesday, April 15, 6 - 7 p.m. Speakers are Rep Caraveo (Legislator and Pediatrician) and Eric France (CDPHE CMO) |
|
Virtual visit tools - Israeli hospital treats Coronavirus patients virtually in their homes (video) |
|
Restarting America will put human lives at risk - The Times Magazine talked to five experts on the ethics of the decision |
|
DEA decision tree (download) |
Resources for Patients
|
|
Mental Health Colorado - FREE resources for self-care |
| Wall Street Journal - What to Put in a Covid-19 Emergency Home-Care Kit |
|
HealthFlix - a series of free online classes from international leaders in health, wellbeing, psychology and lifestyle, designed to help us all cope in this time of global crisis and beyond. |
Key Resources |
|
Colorado Department of Public Health & Environment COVID-19 |
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
April 8, 2020
CPS COVID-19 Resources - April 8th 2020 - Resilience: finding meaning and challenging reality with unity and ingenuity
Do you have a question, helpful resource, or tip for your colleagues? Email [email protected]
Dear Colleagues,
On a recent walk through the neighborhood my son asked, “When do think people will be able to shake hands with one another without thinking about COVID-19?” In posing a previously unthinkable question, my 11-year old touched on a singularly bizarre aspect of this pandemic that distinguishes it from most other calamities in history: our need to ensure physical distance from one another, even those we love. Last week I wrote about physicians and other healthcare workers making the gut-wrenching choice to separate from loved ones. This week, I too have begun that separation. Despite the physical distance (or perhaps because of it), I am learning to find meaning in this strange touchless world. Although it seems a distorted and upside down version of my prior life, I now know that loving someone can mean staying away from them - and finding new and ingenious ways to love and appreciate them from afar. Early morning walks (albeit six feet apart), FaceTime cocktails and good night wishes are now the fabric of my life. Others in my profession have also written about how disconnection can invigorate connection (see CPS Member Kartiki Churi's article).
In his book, Man’s Search For Meaning, psychiatrist Dr. Viktor Frankl noted that human beings can survive almost anything if they find meaning in their suffering. A Holocaust survivor, Dr. Frankl, imagined himself giving lectures on his experience during the Holocaust while at the same time enduring the daily struggles that permeated his life in the camp. In her May 2002 Harvard Business Review article entitled “How Resilience Works,” Diane Coutu quoted, “More than education, more than experience, more than training, a person’s level of resilience will determine who succeeds and who fails. That’s true in the cancer ward, in the Olympics and its true in the boardroom." Ms. Coutu posited that there are three characteristics that make up resilience (whether it be in an individual or an institution): acceptance of reality (without false optimism), a deep belief that life is meaningful and what she described as “an uncanny ability to improvise.” Although written almost twenty years ago, this sums up what it will take for us to survive the ravages of COVID-19 in our personal and professional lives.
Acceptance of reality (or not?)
It’s sobering to think of the reluctant initial response of our government (and perhaps our own personal reactions) to COVID-19. But as we have learned, the world changes on a dime. The harsh reality is a deluge of critically ill patients, whose physicians are forced into making life and death decisions, all the while fearing for their own safety. We hear on a daily basis about lack of PPE and shortages of essential equipment such as ventilators and now of medications that are needed in order to safely ventilate patients. We have to arm ourselves with information (see JAMA article The COVID-19 Pandemic in the US: A Clinical Update) and let facts be our weapons, even when others wish to deny them. Several of you have written to me and expressed concern that your own facility has lagged behind in accepting the necessity of telepsychiatry and masking of staff, and reluctance to accept ideas of how to decrease infection risk. This is not the sort of reality we should accept. In its condemnation of the firing of Dr. Ming Lin, of Bellingham, WA, for taking his concern about lack of PPE to social media after hospital administration failed to respond to repeated requests, the American Academy of Emergency Medicine wrote, “it is an essential duty of a physician to advocate for the health of others.”
Meaning and ingenuity
A call to action during this time of crisis applies not only to physicians who are working in emergency rooms and intensive care units. It applies to all physicians (see YouTube video: Stop Silencing Doctors: a clinical manifesto). In addition to speaking out against injustices in other areas of medicine, we have got to advocate for our patients. Our time for action is now. Our knowledge, experience and beliefs are important. There will be a tsunami of mental illness in the wake of the COVID-19 pandemic, and we must develop safe and effective ways to deliver behavioral health care. The way in which we practice psychiatry has changed at warp speed, and therein are some beautiful examples of ingenuity: an Israeli hospital developed an inpatient unit for psychiatric patients with COVID-19 that is managed on an almost exclusively virtual platform, both Peakview Behavioral Hospital and Centennial Peaks have units for psychiatric patients with COVID-19 (see below), and the APA held a well-informed webinar on caring for such patients (also see JAMA Addressing the COVID-19 Pandemic in Populations With Serious Mental Illness psychiatry). In terms of assisting our fellow physicians, CPS and CMS are holding a webinar this Friday on physician wellness during the crisis and the Colorado Physicians’ Health Program (CPHP) has already set up a helpline (720-810-9131) for doctors who are trying to manage their own fears and anxieties as they treat individuals with COVID 19. Last week Governor Polis issued executive order 20-E-05 requiring carriers to reimburse providers for provision of Telehealth services including those that are solely audio-based. We need more of these examples.
We did not choose this pandemic. But we can choose how we react to it. Knowing what to accept or not is the first step. From there, what is required is the deep belief that life is meaningful and adopting an uncanny ability to improvise. As I told my son, “When else in history would we have been so thoughtful about what we value in life, the people we love and how to connect to them?"
Patricia Westmoreland MD
President
Colorado Psychiatric Society COVID-19 Resource List
April 8, 2020
Updates |
|
|
|
Highlights: The purpose of this emergency regulation is to require carriers to reimburse providers for provision of telehealth services using non-public facing audio or video communication products during the COVID-19 nationwide public health emergency. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Food pantry schedule - A listing (download) of over 30 Denver food pantries with hours and contact information. Call 211 to locate additional resources or to confirm information is current. |
|
|
|
|
|
|
|
Key Resources |
|
|
The references and documents compiled here have been provided by members of CPS and other sources. They are offered as samples for your reference only and are not intended to represent the best or only approach to any particular issue. CPS has not attempted to evaluate any posted material. Neither CPS nor the individuals briefly reviewing the materials make any guarantee with regard to the accuracy of any document, and they assume no responsibility or liability in connection with the use or misuse of any material. Copyright in posted materials belongs to the respective owners, whether or not a copyright notice appears on the screen displaying the materials.
April 7, 2020
If you are interested in COVID-19 volunteer opportunities, please see the information below.
Thank you for your interest in volunteering during the COVID-19 crisis.
CPS is grateful to have members like you who are willing and able to share your time and expertise!
Do you have a question, helpful resource, or tip for your colleagues? Email [email protected]
Colorado Psychiatric Society COVID-19 Resource List
April 3, 2020
Please note links and opportunities are provided as a convenience and do not imply endorsement, legal or financial advice. Users should seek appropriate accounting, legal or other professional advice to address specific facts and circumstances
|
|
State of Colorado COVID-19 Response - We are looking for volunteers to help at-risk individuals across our state get through the COVID-19 crisis. Complete the physician form to be matched with the needs of hospitals, testing sites, or care facilities. |
|
In the coming days, the Colorado COVID-19 Innovation Response Team -- organized by Gov. Jared Polis -- will introduce a telehealth/telemedicine service providing support to ~800,000 uninsured and under-served Coloradans. Their goal is to provide health services while reducing strain on Colorado health care facilities, leaving hospital beds open to the most severely ill. Medical Professionals for Covid-19 Telehealth Response in Colorado - Complete the form if you are interested in volunteering for clinical, triage, or administrative efforts in Colorado. *ALL VOLUNTEER WORK WILL BE REMOTE FROM HOME*. They will reach out to introduce you to the project, and if you are interested in moving forward, will onboard you with a local free clinic so that you are covered by their malpractice insurance. They urgently need medical professionals and administrators to donate their time to provide these free telehealth visits. This work will be performed entirely from home, primarily via telephone and/or video calls. Callers will provide their symptoms over the phone, and those who need medical attention will be triaged to a queue for telephone-based care. More information here.
|
|
CPS has additional opportunities--such as reviewing materials for the CPS COVID-19 Resource Emails--available. Email [email protected] if you are interested in serving in a non-clinical role or if you have another idea for supporting members. |
|
|
|
|
Highlights: Question: Do I still need to contact DORA to obtain some type of provisional license, or can I just start volunteering at healthcare facilities without a Colorado license if I fit the exemptions or suspended rules/statutes? Answer: Under the emergency measures taken by the Division of Professions and Occupations, health care professionals wanting to re-enter the workforce do not need to contact the division or obtain a provisional license provided the following conditions are met:
|
|
Highlights: Q: How can I check if my license is up to date? A: You can verify your licensure status here. However, the State of Colorado issued a release that announced emergency measures for licensure, that allows for individuals with licenses in other states in good standing and retired individuals with current inactive status to be able to practice in the State of Colorado. These updates will not be reflected in the portal. |
|
|
April 1, 2020
Do you have a question, helpful resource, or tip for your colleagues? Email [email protected]
Dear Colleagues,
Another week has gone by and it seems like a month. During this time we have seen our country receive the auspicious designation of number one in Coronavirus cases worldwide with a third of those cases occurring in New York. Two-thirds of the country is now locked down. Worldwide, although the number may be different, the trend and the restrictions are similar.
For me, these last few weeks have been a reminder to appreciate the beauty of life during my early morning runs around the neighborhood, knowing that in my country of origin (South Africa) such sojourns are currently forbidden. I am also grateful that I have a home in which to shelter – and that my engagement in spring cleaning has led to the discovery of childhood mementos. Sharing these treasured items with my children has made our relationship closer, as have our daily walks and discussions as we share household chores (i.e. I clean the guinea pig cage while my daughter watches…a refrain that I am sure many parents will understand). I have also learnt to socialize virtually, reminding my introvert friends to put down their books and check on us extroverts – as the meme goes, “we are NOT okay with this.” In addition, although I am currently seeing patients via telepsychiatry, I know that those days are numbered and once I begin inpatient work again I will very likely have to make the heart-wrenching decision that many of our colleagues have already made (see NYT Opinion article Doctors Are Writing Their Wills): living separately from my significant other and my children. And updating my will. Sobering to think of this, but it has very quickly sharpened my focus on what is important to me: my family (including those family members with four legs), and my commitment to advocating for the safety and welfare of our patients and colleagues.
We hear the outrage from our colleagues in New York and elsewhere regarding lack of PPE and shortage of other essential equipment. Physicians and other health care professionals who have spoken out about the condition in their hospitals are being muzzled and, in some instances, threatened with disciplinary action (see Bloomberg and Kevin MD articles). This is happening not only in emergency rooms and medical units, the frontline for COVID-19, but also in some behavioral health units. Absent a clear dictum for how we manage patients with mental illness through this crisis, facilities have adopted various approaches, with each hospital system apparently developing its own plan as to how to streamline admissions, maximize virtual care, and isolate positive patients. I believe history will judge harshly those who continue to place profit before safety of patients and staff, and we have a duty to speak out against such practices when we see them.
Thankfully, the actions of many institutions have been laudable: numerous entities have been quick to embrace telepsychiatry in order to mitigate exposure of their staff members to potentially positive patients – and vice versa. Many hospitals and behavioral health units have also adopted the strategy of masking all staff members – and in some cases, patients, too. In addition, with a reduced number of admissions many psychiatric units are in a better position than they would previously have been to promote social distancing. Although I don’t by any means have all the answers to this, I do think that reaching out to our colleagues in facilities around the country is useful. To this end I am including a document sent by a colleague at Mt. Sinai and I am also hoping that you will register for (or watch the recording of) the APA’s webinar on inpatient psychiatry. I am also including a link for Peakview Behavioral Hospital, which has opened a unit dedicated to COVID-19 positive patients.
In addition to providing links for telepsychiatry, resources for inpatient admission (although they be disparate and currently scattered), how else can we assist our colleagues, ourselves and our patients?
I invite you to attend townhall meetings and other virtual events with the house of medicine in our state. I think we may need to draft our own letter in the coming weeks detailing the resources we will need to manage the psychological effects of this pandemic not only on our patients but on healthcare providers. In terms of assisting our fellow professionals, CPHP has already set up a helpline (720-810-9131 - additional information below). I, too, need help in the form of hearing from you about the struggles you are faced with in providing care to your patients during this time and how you are managing to take care of your own mental health and that of your family and loved ones. After all, psychiatry is about detailing the experience of humanity in stories, we all have stories to tell, some uplifting, others sobering and yet more filled with humor and hope. As my cousin, an artist herself, posted: “Writers! You have the most incredible story unfolding before your eyes. Take copious notes, and let your imagination soar.” I am hopeful that, in sharing our stories and our resources we will be instrumental in the creation of some positivity in this strange new world.
Patricia Westmoreland MD
President
Colorado Psychiatric Society COVID-19 Resource List
April 1, 2020
Updates |
|
COVID-19 Care Line for Physicians 720-810-9131 |
|
Register here for the Physicians' town hall on COVID-19: Wednesday, April 1, 6 - 7 p.m. with special guest speakers U.S. Sens. Michael Bennet and Cory Gardner |
|
DEA, FTC Issue Warning: Beware of Scammers Be aware: Scammers posing as representatives from the Drug Enforcement Administration (DEA) and officials from other agencies are targeting physicians. It was recently brought to the attention of the Massachusetts Board of Medicine that Massachusetts licensees have been receiving scam calls from individuals posing as investigators of the Massachusetts Board of Medicine of the DEA. In these cases, the impersonator falsely stated that the licensee is under investigation and that their medical license is in jeopardy or has been suspended. Impersonators may demand money and/or seek additional information about the licensee’s DEA registration number and financial information. Physicians from other states received similar scam calls from individuals purporting to be FBI and DEA. The DEA webpage includes information for reporting the threat online. |
Key Resources |
|
Colorado Department of Public Health & Environment COVID-19 |
Resources for Providers
|
|
APA and SAMHSA - Request a Free Clinician-to-Clinician Consult - Mental health professionals can submit questions about COVID-19 and bipolar disorder, major depression, and schizophrenia and receive evidence-based guidance from SMI Adviser's team of national experts within a day. Ask about medications, resources for families, telehealth options, and much more. This is a completely confidential and free service. |
|
Joint APA and NABH Webinar: How to Address COVID 19 Across Inpatient, Residential and other Non-Ambulatory Care Settings Wednesday, April 1, 2:00-3:00 pm (EDT) |
|
Peak View Behavioral Health in Colorado Springs has opened a dedicated unit for presumptive positive COVID patients in need of mental health treatment. This unit is accepting patients effective Thursday, March 26, 2020. This unit will be staffed with specialized dedicated team members. The unit will accept adults and medically-stable older adults and will include medication management, therapy, vitals monitoring, additional medical oversight, and virtual family meetings. |
|
How to Lead through a crisis (download) |
|
Virtual field trips. You can visit over 500 museums, Yellowstone National Park, or even the Great Wall of China. |
|
Humor - MASH and the coronavirus video |
|
Colorado Medical Society Webinar: Limiting the Financial Impact on You and Your Practice - Friday, April 3, 12 - 1 pm - Register for this Friday's midday webinar for more information on financial assistance available to your practice |
|
Survey Finds COVID-19 Takes Heavy Psychological Toll on Health Care Workers - http://alert.psychnews.org/2020/03/survey-finds-covid-19-takes-heavy.html |
|
MD Edge - Psychiatrists deemed ‘essential’ in time of COVID-19 and response |
Resources for Patients
|
|
American Academy of Pediatrics - Talking to and Supporting Children During a Pandemic - This webinar discusses effective communication strategies for clinicians in general and specifically ways to talk to and support children during the COVID-19 pandemic. Strategies to help parents communicate with their children are also included. |
|
World Health Organization Coronavirus disease (COVID-19) advice for the public: Myth busters |
|
|
Psychiatrists Needed for Clinical Relief Medical personnel on the front lines are quickly becoming overwhelmed. If you are able to cover essential services for psychiatric emergency services, inpatient units, methadone centers, jails and other settings, Denver area hospitals and other facilities will emergency credential and train psychiatrists. If you are interested, please email your name and skills to [email protected] with "ESSENTIAL" in the subject line. Note: Contact your professional liability insurance carrier to confirm if they cover you for the rendering of psychiatric services as a volunteer in the state where you are licensed. Question: Do I still need to contact DORA to obtain some type of provisional license, or can I just start volunteering at healthcare facilities without a Colorado license if I fit the exemptions or suspended rules/statutes? Answer: Under the emergency measures taken by the Division of Professions and Occupations, health care professionals wanting to re-enter the workforce do not need to contact the division or obtain a provisional license provided the following conditions are met:
|
|
Urgent: Volunteer to provide free telehealth visits In the coming days, the Colorado COVID-19 Innovation Response Team -- organized by Gov. Jared Polis -- will introduce a telehealth/telemedicine service providing support to ~800,000 uninsured and under-served Coloradans. Their goal is to provide health services while reducing strain on Colorado health care facilities, leaving hospital beds open to the most severely ill. They urgently need medical professionals and administrators to donate their time to provide these free telehealth visits. This work will be performed entirely from home, primarily via telephone and/or video calls. Callers will provide their symptoms over the phone, and those who need medical attention will be triaged to a queue for telephone-based care. More information here. |
March 25, 2020
CPS Resource list is below the Message from the President
To see past resource lists, messages, and articles, click here
Do you have a question, helpful resource, or tip for your colleagues? Email [email protected]
Dear Colleagues,
I can’t believe that it’s only been a week since I first wrote you, hoping to provide resources you might find useful as we band together (albeit at a social distance) in our fight against COVID-19. Since then, it’s been a week of restaurant, store and business closures. Though some of these businesses are labeled ‘non-essential’ they are all but that for the workers whose livelihoods depend on them. In addition, one in four Americans has been ordered to shelter in place. For those of us not yet in this position, the rhythm of our day to day lives has been severely disrupted. Yet, as we grapple with our own grief at the loss of life as we knew it, as well as the fear of further loss, we are forced to get our act together in a hurry to protect and care for our families and our patients. We also need to maintain our strength and sanity as we learn to adapt to this strange new world.
In my interactions both with members of our psychiatric community in Colorado as well as around the country, I have found an overwhelming thirst for knowledge and discourse as we scramble to find our way forwards. It has been sobering to find that our virtual meetings have run hours longer than expected as we share information about COVID-19 and find ways to help each other. Here’s what’s come up this week:
Telepsychiatry
Many of you have already been using telepsychiatry in your practices previously. Rules and regulations regarding the use of telehealth in total (and telepsychiatry in particular) have evolved rapidly over the last week. Some of the changes include lifting of restrictions regarding HIPAA compliant modalities and seeing patients across state lines, and CMS mandated changes in billing (with many insurance companies following suit).
Inpatient psychiatric facilities and correctional facilities
While telepsychiatry has been useful in the outpatient setting, some facilities are using it for partial hospital, residential and inpatient care, although there may be greater logistical difficulties in its implementation. Nonetheless, patient check ins, rounding and treatment team meetings may still be accomplished virtually, thus enabling us to adjust medication, provide counsel and exchange information all the while reducing exposure. That being said, for many institutions the mere act of getting the patient in front of the virtual setting may prove cumbersome and take up additional staff time. In addition, there are some tasks and procedures that require physician presence (ECT, ketamine infusion). Perhaps having physicians attend in person on a rotating schedule (and exempting those at high risk from direct patient contact altogether) may be useful - suggestions welcome! But what do we do to prevent COVID-19 from taking hold in an inpatient unit and killing our patients as it did in a psychiatric unit in South Korea? Dr. Dinah Miller’s article in MD Edge Psychiatry details concerns particular to inpatient units and our treatment of acutely psychiatric patients and provides some preliminary thoughts and guidance. However, many of us are still grappling with the peculiarities of our local situation and how each hospital chooses to identify and isolate potential COVID-19 cases and protect their staff - or not.
While the sobering piece by Dr. Hylton is written from the perspective of a pediatric ER doctor, her statements apply to us, too. As Dr. Hylton writes, some hospital administrators “emboldened by the lack of consistency in the CDC’s guidelines are insisting that masks and PPE are unnecessary for all but certain high-risk procedures and patients.” Ignoring the potential for widespread community spread through asymptomatic individuals, some facilities have expressly forbidden front line staff from wearing PPE in the name of “not scaring the patient” even if they are able to procure such equipment from a third party source. This issue has been discussed with APA leadership, and it is likely that local and state government involvement will be required to address this concern.
Concern for the psychological effects of COVID-19
We likely all experienced our profession being the forgotten stepchild of medicine. Now is no different. There are few if any media reports about psychiatric illness and even less consideration as to how patients, already mentally fragile, are coping with a new and troubling reality. According to my APA colleagues in the State of Washington, there is already an increase in domestic violence and substance use (even in those who had maintained sobriety for an extended period of time). Individuals with eating disorders are particularly vulnerable as they suffer both the mental and physical stigmata of their illnesses. Dr. Jennifer Gaudiani provides us with an excellent outline of her concerns regarding COVID-19 and eating disorders. I will be providing more information on the effects of COVID-19 on our patients in future communications. If you have articles you would like us to share, please send them to [email protected].
I do believe that we will see a greater need for mental health care as our new “normal” emerges, so let’s continue our virtual banding together and keep each other strong and help each other move forward. Thank you to my colleagues on the CPS Executive Council, Area 7 and the APA for their ideas and discourse.
Patricia Westmoreland MD
President
Colorado Psychiatric Society COVID-19 Resource List
March 25, 2020
Key Resources |
|
Colorado Department of Public Health & Environment COVID-19 |
|
|
U.S. Dept. of Health & Human Services (HHS) - Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency |
|
Health First Colorado: https://www.colorado.gov/pacific/hcpf/provider-telemedicine |
|
|
Register here to join the Colorado Medical Society for a virtual town hall meeting on COVID-19 on Wednesday, March 25, 6 - 7:30 p.m. Just like the first CMS-hosted town hall on March 18, physicians will engage directly with key stakeholders to get support and answers on this pandemic. Panelists: Eric France, MD, MPH (Chief Medical Officer at Colorado Department of Public Health and Environment); Gretchen Hammer (Founder, Public Leadership Group and current member of the State of Colorado Innovation Response Team); Lisa Latts, MD, MSPH, MBA, FACP (CDPHE Chief Medical Officer); Melanie Simons (CDPHE Public Health Emergency Preparedness/Medical Countermeasures Program Manager) Note: Participation is capped at 500. Those unable to join live will be able to watch an archived version on CMS.org. Additional town halls will be held Wednesday evenings for the foreseeable future. |
|
|
Surreal Boundary Shifts During a Pandemic by Claire Zilber, MD March 2020 |
|
U of Colorado Anschutz Medical Campus - Health Care Provider Well-Being During Covid-19 |
|
APA/SAMHSA - free webinar on Telepsychiatry in the Era of COVID-19 |
|
CPHP - Resources to Promote Well-being During COVID-19 Outbreak |
|
Headspace - US healthcare professionals who work in public health settings get free access to Headspace Plus through 2020 |
|
AMA Journal of Ethics Podcast » Ethics Talk: COVID-19 Pandemic Response - Listen now |
|
The psychological impact of quarantine and how to reduce it: rapid review of the evidence (Lancet, Rapid Review) |
|
APA Coronavirus and Mental Health: Taking Care of Ourselves During Infectious Disease Outbreaks Highlights: |
|
|
CPHP - Comprehensive list of general resources for coping with the current COVID 19 situation in CO |
|
Google Arts & Culture teamed up with over 500 museums and galleries around the world to bring anyone and everyone virtual tours and online exhibits of some of the most famous museums around the world |
|
“FACE COVID” (Dr. Russ Harris, author of The Happiness Trap) - Practical steps based on Acceptance & Commitment Therapy F = Focus on what’s in your control C = Committed action |
|
National Child Traumatic Stress Network: Parent/Caregiver Guide to Helping Families Cope With the Coronavirus Disease 2019 (COVID-19) – Common reactions by age group and the best ways to respond |
|
|
Survey on Impact of Coronavirus on Mental Health Care Dear psychiatric colleague, We are trying to understand how mental health providers are receiving information and altering care practices in response to the coronavirus SARS-CoV-2 (aka COVID-19) epidemic. Please take less than 10 minutes to complete this survey: https://dhharedcap.ucdenver.edu/surveys/?s=WF8EPCKD8K This study has been reviewed by the Colorado Institutional Review Board (www.ucdenver.edu/research/comirb) or 303-724-1055. Thank you for all that you do, Scott Simpson MD MPH, Medical Director, Psychiatric Emergency Services, Denver Health Medical Center, [email protected] |
|
Psychiatrists Needed for Clinical Relief Medical personnel on the front lines are quickly becoming overwhelmed. If you are able to cover essential services for psychiatric emergency services, inpatient units, methadone centers, jails and other settings, Denver area hospitals and other facilities will emergency credential and train psychiatrists. If you are interested, please email your name and skills to [email protected] with "ESSENTIAL" in the subject line. Note: Contact your professional liability insurance carrier to confirm if they cover you for the rendering of psychiatric services as a volunteer in the state where you are licensed. |
March 16, 2020
Dear Dr. ,
As President of CPS I have heard from many of you in response to the rapidly evolving developments surrounding the spread of COVID-19. I am concerned about the impact of this pandemic on my family, my patients and the more vulnerable members of our society. How we protect those we hold dear? How do we honor our obligations to the patients we care for? How do we minimize the risk of becoming ill ourselves? Minds wiser than mine have pondered these issues, and sadly countries other than our own have grappled with the consequences of not being prepared - let’s hope we can learn from these lessons.
As we all scramble to wash our hands more frequents and practice social distancing, I think it’s important to remember that it is now in this time of crisis that we as human beings need each other more than ever. As a social person I am disappointed in the cancellation of meetings as well as social gatherings. I enjoy exchanging ideas with others as well as interaction on a personal basis. Nonetheless, I strongly believe it is our moral obligation to carefully evaluate our travel plans, stay put and minimize the risk not only of getting infected ourselves, but passing COVID-19 to others, especially those who are vulnerable in our society. To this end I am sharing a Newsweek article that has been distributed on the APA Area 7 and Assembly listservs as well as by an ID colleague whose work I greatly respect. I sincerely hope that by delaying the gratification we all feel will help us “flatten the curve” and reduce the impact of COVID-19 on our healthcare system.
Speaking of which – what is like to care for patients with COVID-19? Dr. Brooke Parish, MD, New Mexico Representative to APA gave me permission to share with you her beautifully articulated piece regarding her experience in caring for individuals with COVID-19. Dr. Parish, who is also an internist, traveled to Lackland Air Force Base several weeks ago to care for patients from the Diamond Princess.
Along with our CPS Executive Council and our Disaster Representative Scott Simpson, I am monitoring the rapidly evolving situation. While we do not want to be duplicative, in response to member requests, we have compiled a list of resources that may be helpful (attached). Many of you have asked about the role telepsychiatry will play. To this end we have included information from PRMS as well as the APA. Please contact us if we can be of further assistance. Best wishes for your continued health and safety.
Patricia Westmoreland MD
CPS President
CPS COVID-19 Resources 3-13-2020(2).docx
Physician Mental Health During COVID-19: A Call to Action dece